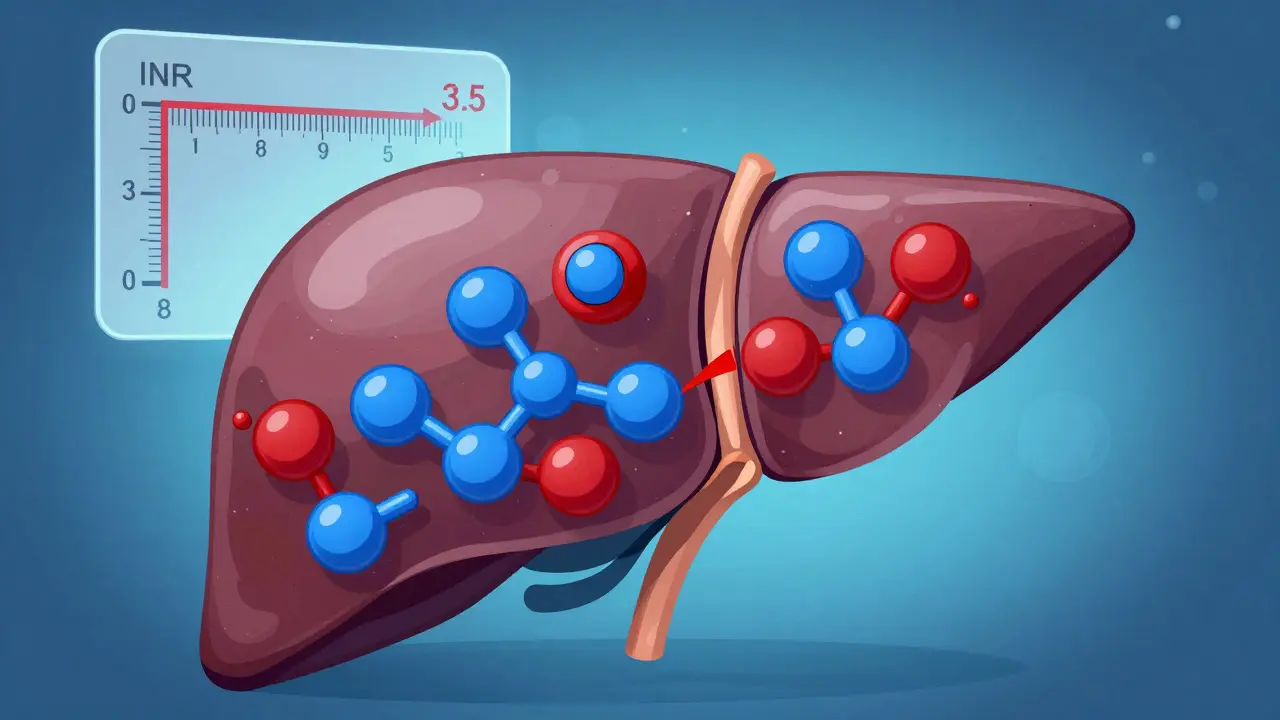
INR Risk Calculator
Assess Your Alcohol & INR Risk
Based on current INR value, alcohol intake, and genetic factors
Your target range is typically 2.0-3.5 for warfarin patients
1 unit = 12g alcohol (approx. 125ml wine, 350ml beer, 25ml spirits)
When you're on a blood thinner like warfarin, even a weekend drink can throw your blood off balance. It’s not just about getting drunk-it’s about how alcohol quietly messes with your INR, the number that tells your doctor if your blood is clotting too slowly or too fast. And when that number spikes, the risk of serious bleeding goes up fast. You might think, "I only have one glass of wine," but that one glass can be enough to push your INR into dangerous territory, especially if you're not watching your intake closely.
What Is INR, and Why Does It Matter?
INR stands for International Normalized Ratio. It’s a blood test that measures how long it takes your blood to clot. If you’re not on blood thinners, your INR is usually between 0.8 and 1.1. But if you’re taking warfarin, your target range is between 2.0 and 3.5-depending on your condition. For atrial fibrillation, it’s often 2.0-3.0. For a mechanical heart valve, it might be 2.5-3.5. Stay within that range, and you’re protected from clots without bleeding too much. Go above 3.5, and your risk of internal bleeding jumps. Above 9? That’s a medical emergency.
Every 0.5-point rise above your target INR increases bleeding risk by 30-50%. That’s not theoretical. In one study, 11% of outpatients with INR over 9 had a bleeding event. In hospitalized patients? 35% bled, and 17% died. Alcohol is one of the top three reasons those numbers climb-alongside older age and kidney problems.
How Alcohol Messes With Warfarin
Warfarin doesn’t work the same way as newer blood thinners like apixaban or rivaroxaban. Those drugs have fewer interactions. Warfarin? It’s finicky. It’s broken down in your liver by enzymes that alcohol also affects. When you drink, especially in large amounts, your liver gets busy processing alcohol instead of warfarin. That means warfarin sticks around longer, making your blood thinner than intended.
But here’s the twist: it doesn’t always work the same way. Sometimes alcohol makes warfarin less effective-especially if you drink regularly. Your liver gets used to processing alcohol and starts breaking down warfarin faster. That can drop your INR, putting you at risk for a clot. Then you stop drinking for a few days, and suddenly your INR spikes. It’s a rollercoaster. And your doctor can’t predict it just by looking at your chart.
Studies show that even moderate drinking-two or three drinks in a weekend-can cause INR fluctuations big enough to require a warfarin dose change. One patient in Australia saw his INR jump from 2.4 to 3.8 after four glasses of wine. His doctor told him it was common. It was. But it didn’t have to happen.
Alcohol and Genetic Risk: It’s Not the Same for Everyone
Not everyone reacts the same way to alcohol and warfarin. Your genes play a role. Two specific gene variants-CYP2C9*2/*3 and VKORC1 1173G>A-make your body process warfarin differently. If you have them, even small amounts of alcohol can cause dangerous INR spikes. A 2015 NIH study found that people with these variants had a much higher risk of major bleeding when drinking, especially if they’d been on warfarin for over a year.
That means two people drinking the same amount could have totally different outcomes. One might be fine. The other could end up in the ER with internal bleeding. There’s no easy way to know your genetic risk without a test. But if you’ve had unexplained INR swings in the past, or if you’ve had a bleeding event after drinking, your doctor might consider genetic testing.

What Counts as "Too Much" Alcohol?
The guidelines aren’t complicated, but they’re strict. The British Heart Foundation and NHS both say: if you drink, stick to the low-risk limits. That’s no more than 14 units of alcohol per week-spread over three or more days. One unit is about half a pint of beer, a small glass of wine, or a single shot of spirits.
Heavy drinking? That’s more than 14 drinks a week for men, or 7 for women. Binge drinking-even one night of six beers or five glasses of wine-is especially dangerous. It causes sudden, unpredictable spikes in INR. One man in Melbourne had a GI bleed after six pints of beer. His INR went from 2.8 to 5.2 in under 48 hours. He needed a hospital stay. He didn’t need to drink that much.
Consistency matters more than occasional drinking. If you drink one glass of wine every night, your body adjusts. Your INR stays more stable. But if you go from zero to six drinks on Friday, then none all week, your INR swings wildly. That’s the real danger.
What About Newer Blood Thinners?
If you’re on apixaban, rivaroxaban, dabigatran, or edoxaban-these are called DOACs-you don’t need regular INR tests. They’re less affected by alcohol than warfarin. But that doesn’t mean you’re safe. Heavy drinking still increases bleeding risk, even on DOACs. Alcohol thins your blood on its own. Add it to a blood thinner, and you’re doubling down on the effect.
And here’s the catch: if you bleed on a DOAC, there’s no quick fix like vitamin K or plasma infusion. For warfarin, doctors can reverse the effect. For DOACs? Sometimes they can’t. So while DOACs are easier to manage, they’re not risk-free with alcohol.

Signs You’re Bleeding-Don’t Ignore Them
Internal bleeding doesn’t always look like a cut. It can be quiet. Watch for:
- Red or brown urine
- Tar-like or bright red stools
- Bleeding gums or nosebleeds that won’t stop
- Unusually heavy periods
- Brown or bright red vomit
- Unexplained bruising, especially large patches
- Severe headaches, dizziness, or weakness (could mean brain bleed)
If you notice any of these-and you’ve been drinking-call your doctor or go to the ER. Don’t wait. Bleeding from warfarin can be silent until it’s life-threatening.
What Should You Do?
You don’t have to quit alcohol entirely-but you do need to be smart about it.
- Keep it moderate. Stick to 14 units a week, spread out. No bingeing.
- Be consistent. If you drink, drink the same amount every time. Don’t go from zero to six.
- Tell your doctor. If you drink, even occasionally, make sure they know. It affects how often you need INR checks.
- Get tested more often after drinking. If you had a weekend of alcohol, ask for an INR test a few days later.
- Don’t mix alcohol with other meds. Painkillers like ibuprofen or even some herbal supplements can increase bleeding risk too.
Some clinics now offer telehealth programs that include alcohol counseling for warfarin patients. One study showed a 25% drop in INR-related complications when patients got this kind of support. It’s not just about the number on the screen-it’s about habits.
Bottom Line
Alcohol and warfarin don’t mix safely unless you’re careful. The risk isn’t just about getting drunk. It’s about the quiet, unpredictable way alcohol changes how your body handles your medication. Your INR is your early warning system. If you drink, treat it like a variable in a math equation-one that can throw off your whole balance.
If you’re unsure, talk to your doctor. Ask: "What’s my target INR?" "How does alcohol affect mine?" "Should I get tested after drinking?" Don’t assume it’s fine. Don’t assume you’re an exception. Warfarin is a powerful tool-but it’s not forgiving. Your safety depends on knowing the rules and sticking to them.


Okay but let’s be real-why are we still talking about warfarin like it’s 2008? DOACs exist for a reason. If you’re drinking and on warfarin, you’re basically playing Russian roulette with your internal organs. I get it, you’re attached to your Friday wine, but your liver isn’t a fan of your nostalgia.
Just switch. It’s not that hard. Your doctor’s probably begging you to.
And no, ‘I’ve been on it for 10 years’ doesn’t count as a valid excuse. Your body changes. Your habits change. Your INR shouldn’t be a weekly horror story.