When you stand up from a chair and feel dizzy, lightheaded, or like you might pass out, it’s easy to blame it on getting up too fast. But if this happens every day - or worse, multiple times a day - it’s not just being clumsy. It could be your autonomic nervous system failing. Autonomic neuropathy is a hidden condition that quietly damages the nerves controlling your heart, blood pressure, digestion, and more. It doesn’t show up on routine blood tests. Many doctors miss it. But for those living with it, the symptoms are brutal: sudden drops in blood pressure, nausea, vomiting, bloating, constipation, and diarrhea that turn everyday life into a minefield.
What Exactly Is Autonomic Neuropathy?
Autonomic neuropathy isn’t a single disease. It’s a collection of symptoms caused by damage to the nerves that run your body’s automatic functions - things you don’t think about, like how fast your heart beats, how your stomach digests food, or how your blood vessels tighten to keep you from fainting when you stand up. These nerves are part of the autonomic nervous system, and when they get damaged, your body can’t respond properly to changes in position, temperature, or digestion.
Most cases - 85% to 90% - are linked to diabetes. High blood sugar over years slowly eats away at the tiny blood vessels that feed these nerves. The result? Nerves starve. They misfire. They stop working. But it’s not just diabetes. Autoimmune disorders, certain chemotherapy drugs, Parkinson’s disease, and even some viral infections can trigger it too. The problem? By the time people feel symptoms, the damage is often advanced. Studies show that up to 70% of people with long-term diabetes have nerve damage, but only about 20% notice symptoms early enough to act.
Why Your Blood Pressure Crashes When You Stand Up
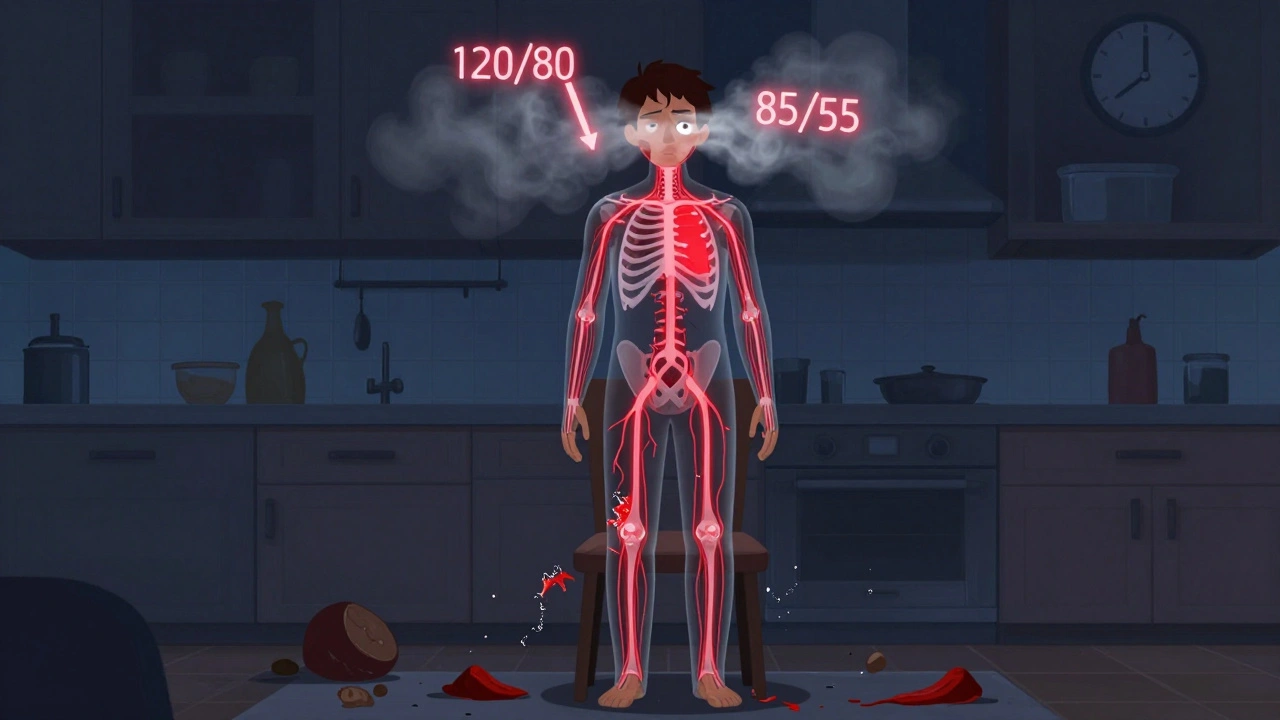
Standing up should be simple. Your body senses the drop in blood pressure caused by gravity and instantly tells your heart to beat faster and your blood vessels to squeeze tighter. That keeps blood flowing to your brain. In autonomic neuropathy, that signal never gets through.
This is called orthostatic hypotension. It’s defined as a drop of 20 mmHg in systolic blood pressure or 10 mmHg in diastolic within three minutes of standing. In severe cases, systolic pressure can plummet from 120 to 85 in seconds. People describe it as their vision going gray, their head spinning, or their legs turning to jelly. Some faint. Others just feel like they’re about to.
Studies show that about 30% of people with diabetic autonomic neuropathy experience this. In one Mayo Clinic study, patients lost an average of 35 mmHg systolic when tilted upright. That’s not just dizziness - that’s a medical emergency waiting to happen. And it’s not just about falling. These drops in blood pressure increase the risk of heart attacks and strokes by more than five times. The heart struggles to pump efficiently because the nerves that control its rhythm are damaged too. Heart rate variability - a key measure of autonomic health - often drops below 1.1 during deep breathing, a clear red flag.
Some people don’t get low blood pressure - they get fast heart rate instead. That’s Postural Orthostatic Tachycardia Syndrome (POTS). When they stand, their heart races past 120 beats per minute, even if blood pressure stays normal. POTS affects 1 to 3 million Americans, mostly young women. While some experts argue it’s a separate condition, most agree it’s part of the same spectrum: damaged nerves, confused signals, and a body that can’t regulate itself.
Why Your Stomach Stops Working
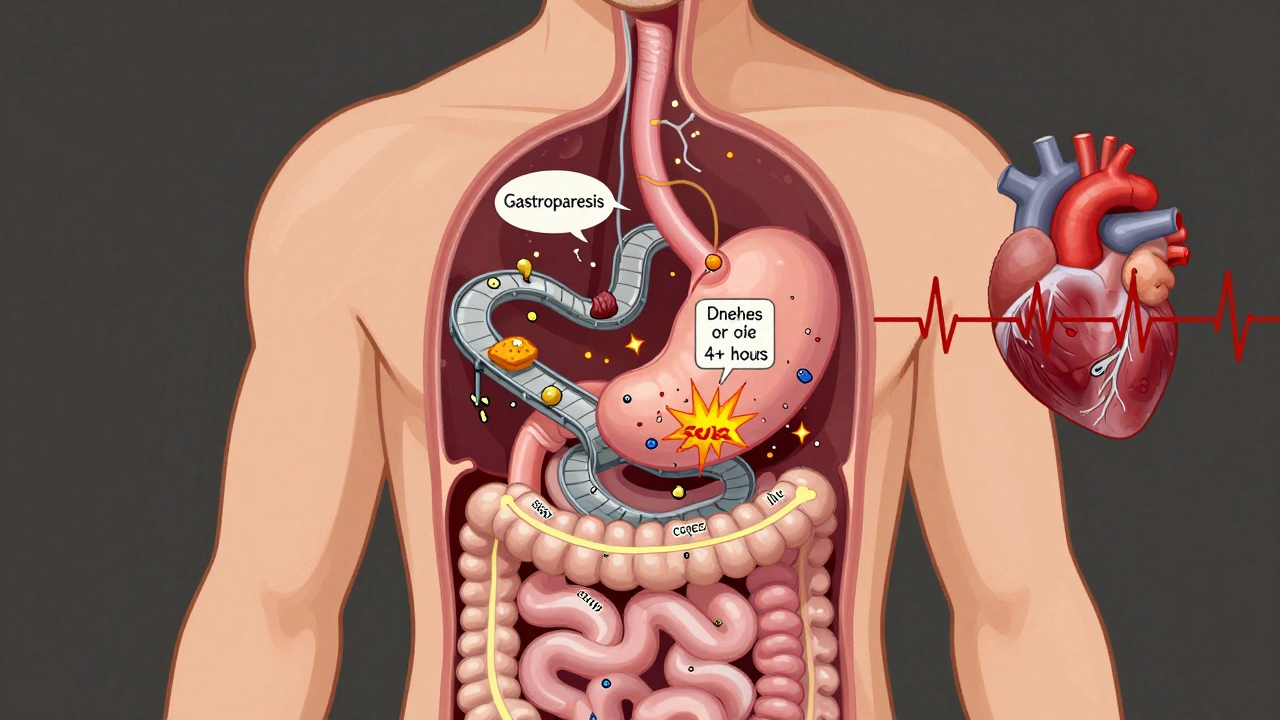
While blood pressure crashes are scary, the gastrointestinal symptoms are often more disabling. Imagine eating a meal and then feeling full for hours. Or vomiting at night, even when you haven’t eaten. Or alternating between constipation and explosive diarrhea. This isn’t IBS. This is gastroparesis - a condition where the stomach doesn’t empty properly because the vagus nerve, which controls stomach contractions, is damaged.
Up to 30% of people with diabetic autonomic neuropathy develop gastroparesis. Scintigraphy tests show that their stomachs still hold more than 10% of food four hours after eating. Normal stomachs empty in under two. The result? Bloating, nausea, early fullness, and vomiting - often at night, when you’re trying to sleep. One Mayo Clinic study found that 78% of these patients vomited at night. Nearly half had symptoms every day.
But it’s not just the stomach. The whole digestive tract gets messy. Constipation hits 60% of patients - some only go once a week. Diarrhea affects 25%, often at night. Many have both, switching back and forth. Why? Because nerves controlling the intestines are damaged too. Food moves too slowly in some parts, too fast in others. This creates a breeding ground for bacteria. In fact, over half of patients with GI symptoms have small intestinal bacterial overgrowth (SIBO), which causes gas, bloating, and diarrhea. It’s a vicious cycle: nerve damage → slow digestion → bacteria overgrow → more symptoms.
Swallowing can also become hard. About 35% of patients have trouble with esophageal motility - the muscles in the esophagus don’t squeeze right. Food gets stuck. It feels like something’s lodged in your chest. That’s another hidden symptom most doctors overlook.
How Doctors Diagnose It (And Why So Many Miss It)
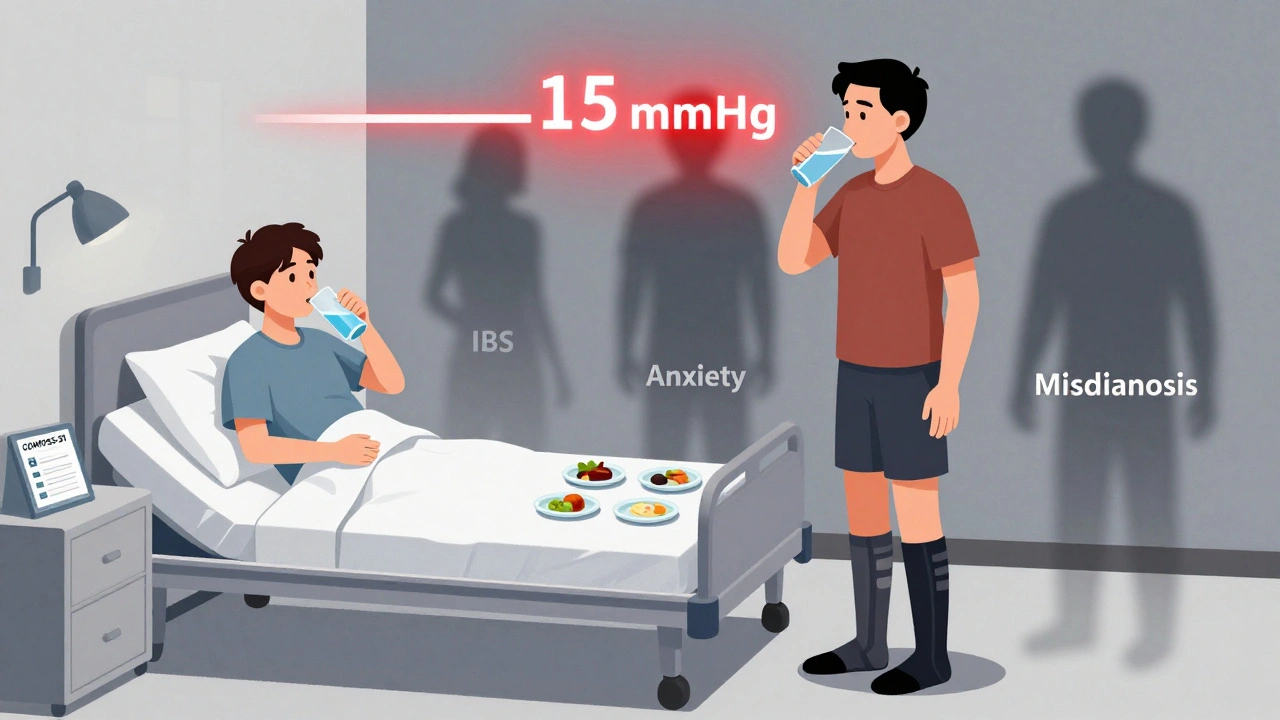
There’s no single blood test for autonomic neuropathy. Diagnosis relies on a mix of symptom reports and objective tests. The simplest is the 10-minute active stand test: measure your blood pressure and heart rate while lying down, then every minute as you stand. A drop of 20 mmHg systolic or 10 mmHg diastolic confirms orthostatic hypotension.
More advanced tests include heart rate variability during deep breathing, the Valsalva maneuver (forced exhalation against a closed airway), and QSART (Quantitative Sudomotor Axon Reflex Test), which checks sweat production. For GI issues, gastric emptying scintigraphy is still the gold standard - you eat a meal with a tiny radioactive tracer, and a camera tracks how fast it leaves your stomach.
But here’s the problem: most primary care doctors don’t think to test for this. A 2021 audit found that only 30% of cases were recognized in routine visits. Patients often see three or more specialists before getting a diagnosis - and wait an average of 4.7 years. That’s years of unnecessary suffering, misdiagnoses as anxiety or IBS, and worsening nerve damage.
New tools are helping. The COMPASS-31 questionnaire scores symptoms from 0 to 100. A score above 30 means significant autonomic dysfunction. It’s fast, reliable, and correlates with real nerve damage. The American Diabetes Association now recommends annual screening for anyone with diabetes for more than seven years - a step forward, but still not routine everywhere.
Treatment: What Actually Works
Treatment isn’t about curing the nerve damage - it’s about managing symptoms and preventing complications. And it’s not one-size-fits-all.
For blood pressure drops:
- Fludrocortisone helps your body hold onto salt and water, increasing blood volume. It works for about 60% of people, but 35% end up with high blood pressure when lying down - dangerous for the heart.
- Midodrine tightens blood vessels. It’s effective for 70% of patients, but you have to time your doses carefully. Taking it too late in the day can cause dangerous supine hypertension.
- Ivabradine slows a racing heart in POTS patients. It cuts heart rate by 15-25 beats per minute in two-thirds of users, without affecting blood pressure.
- Compression garments - especially waist-high stockings - help squeeze blood back up from your legs. In one Mayo Clinic trial, they reduced orthostatic symptoms by 40%.
- Salt and fluids are simple but powerful. Increasing sodium intake to 8-10 grams per day (with doctor approval) and drinking 2-3 liters of water daily can make a huge difference.
For GI symptoms:
- Metoclopramide speeds up stomach emptying, but it carries a black box warning: long-term use can cause irreversible movement disorders like tardive dyskinesia.
- Erythromycin works well short-term, but most people develop tolerance within weeks.
- Pyridostigmine is emerging as a safer, effective option. It improves symptoms in 55% of patients with minimal side effects.
- Diet changes are critical. Eating six small meals a day, avoiding high-fat and high-fiber foods, and choosing easily digestible carbs can cut vomiting episodes in half. One patient reported going from five vomiting episodes a day to one every three days just by changing what she ate.
- Probiotics and FMT are being studied. Early results from fecal microbiota transplants show promise in restoring gut balance and reducing SIBO-related symptoms.
Living With It: Real People, Real Strategies
Reddit threads and patient forums are full of raw, honest stories. One user, 'ChronicWarrior2020,' wrote: 'The moment I stood up, my BP would drop from 120/80 to 85/55 within 30 seconds - fludrocortisone finally gave me 4 hours of upright tolerance.' Another, 'GastroparesisFighter,' said: 'The low-fat, low-residue diet cut my vomiting from five times a day to once every three days - worth every social sacrifice.'
People learn to adapt. They wear compression socks. They sit on the edge of the bed for a minute before standing. They avoid hot showers, alcohol, and large meals. They carry snacks and water. They cancel plans because they don’t know if their stomach will cooperate. One survey found that 89% avoid hot environments, 76% wear compression gear daily, and 68% increase salt intake - all to stay upright, functional, and safe.
The emotional toll is heavy. Anxiety, depression, and isolation are common. The unpredictability makes it hard to work, socialize, or even leave the house. But many find community. Online groups offer support, tips, and validation. For many, the biggest relief isn’t a drug - it’s knowing they’re not crazy, and someone finally understands.
The Future: What’s Coming Next
Research is moving fast. Scientists are now measuring neurofilament light chain levels in blood - a protein that leaks when nerves are damaged. Higher levels mean worse autonomic dysfunction. This could lead to blood tests that catch the disease before symptoms start.
The 2025 American College of Cardiology guidelines will lower the threshold for diagnosing orthostatic hypotension from a 20 mmHg drop to 15 mmHg. That means earlier detection. Earlier intervention. Better outcomes.
Meanwhile, the diagnostic testing market is booming - projected to grow from $185 million in 2023 to over $310 million by 2028. More awareness, more tools, more hope.
But the reality remains: autonomic neuropathy still cuts life expectancy by over eight years in severe cases. It’s not just a complication of diabetes - it’s a life-altering condition that demands attention, research, and compassion.
If you have diabetes and you’re feeling dizzy when you stand, or your stomach won’t digest food, or you’re constantly bloated and constipated - don’t brush it off. Ask for a screening. Push for answers. Your nerves are trying to tell you something. Listen.


So let me get this straight - your body’s like a rusty old car that forgot how to shift gears when you stand up? 🤯 I’ve been told I’m ‘just anxious’ for YEARS until I finally got diagnosed. Now I wear compression socks like they’re fashion statements and chug salt water like it’s my job. Who knew being alive could feel like a glitch in the Matrix?