Every year, thousands of older adults end up in the hospital because of a medication that shouldn’t have been prescribed in the first place. It’s not always a mistake - sometimes it’s just the system working the way it’s designed. But when a 78-year-old with mild dementia is given an antipsychotic to calm agitation, or a 72-year-old with kidney issues is still prescribed a NSAID for arthritis pain, the risk isn’t just theoretical. It’s real. And that’s where the Beers Criteria come in.
What Exactly Are the Beers Criteria?
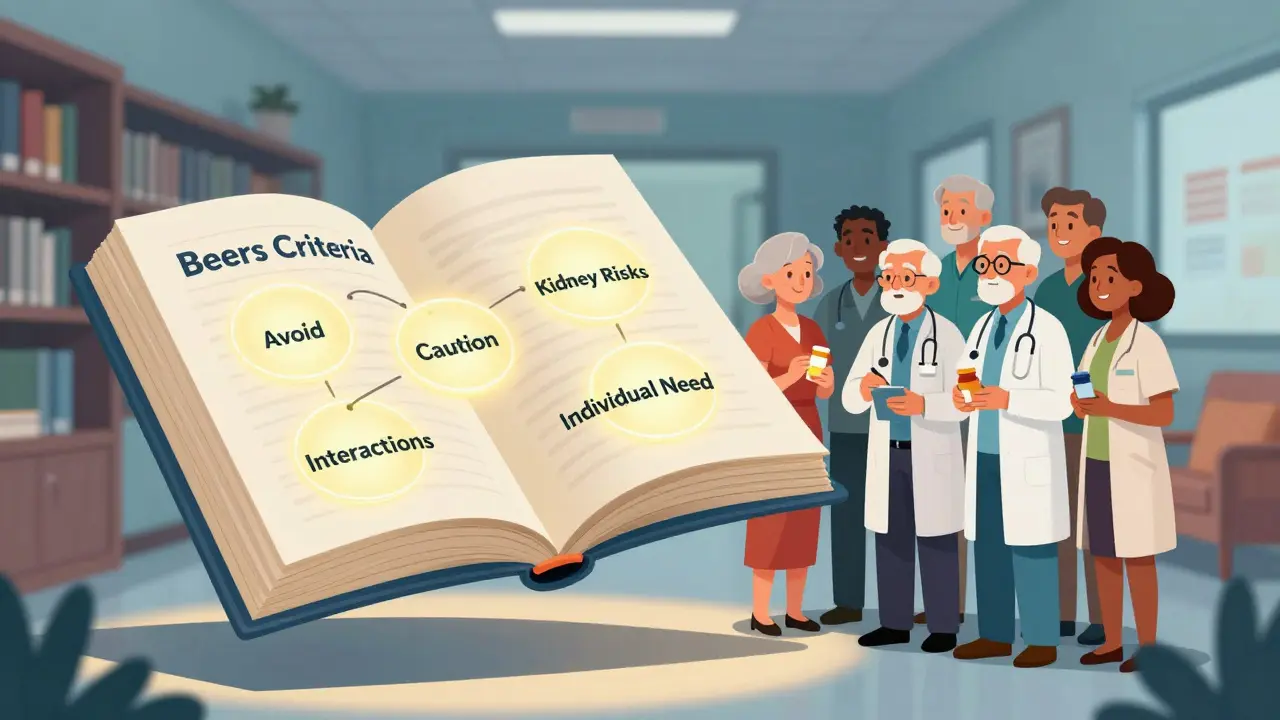
The Beers Criteria are a list of medications that doctors and pharmacists should avoid prescribing to adults aged 65 and older, unless there’s a very clear reason to do otherwise. Developed in 1991 by Dr. Mark Beers and updated every few years by the American Geriatrics Society (AGS), the latest version came out in 2023. It’s not a law. It’s not a blacklist. It’s a warning sign - a practical guide built on decades of research showing which drugs do more harm than good in older bodies.Why do we need this list? Because aging changes how your body handles medicine. Your kidneys slow down. Your liver processes drugs less efficiently. Your brain becomes more sensitive to sedatives. What was safe at 50 might be dangerous at 80. The Beers Criteria help cut through the noise and point out the medications that are most likely to cause falls, confusion, kidney damage, or even death in older people.
The Five Categories of Risk
The 2023 update breaks down 131 specific medication warnings into five clear groups. Here’s what they mean in plain language:- Medications to avoid in most older adults - These are drugs that are rarely worth the risk. Think benzodiazepines like diazepam (Valium), antipsychotics like haloperidol, and certain sleep aids like diphenhydramine (Benadryl). These can cause dizziness, memory loss, and falls. Even short-term use can be dangerous.
- Medications to avoid if you have certain conditions - Some drugs are okay for most people but dangerous if you have specific health issues. For example, nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen or naproxen can cause stomach bleeding or kidney failure in people with high blood pressure or heart failure. Anticholinergics like oxybutynin (for overactive bladder) can make dementia worse.
- Medications to use with caution - These aren’t outright banned, but they need close monitoring. Examples include certain antidepressants (like amitriptyline), proton pump inhibitors (PPIs) taken long-term, and some blood pressure drugs that can drop blood pressure too much.
- Medications to avoid with kidney problems - As kidney function declines with age, many drugs build up in the body. Metformin (for diabetes) and certain antibiotics like gentamicin need dose adjustments or complete avoidance if kidney function is low.
- Drug interactions to avoid - Some combinations are especially risky. For example, mixing an NSAID with a blood thinner like warfarin increases bleeding risk. Combining multiple sedatives (like a sleep aid with an anti-anxiety med) can slow breathing dangerously.
Each of these 131 criteria is backed by research - not opinion. The 2023 panel reviewed over 1,500 studies published between 2019 and 2022. They didn’t just look at side effects. They looked at real outcomes: hospital stays, falls, cognitive decline, and death.
Why This Matters More Than You Think
About 40% of older adults take five or more medications daily. That’s called polypharmacy. And in about 20% of those cases, at least one of those drugs is flagged by the Beers Criteria. That’s not a small number - that’s millions of people.Studies show that when older adults are prescribed a Beers Criteria drug, their risk of hospitalization goes up by 30% to 50%. Falls increase. Confusion gets worse. Kidneys get damaged. And in some cases, people die because of a medication that was never meant to be long-term.
One 2014 study looked at older patients stuck in hospital beds waiting for long-term care - called Alternate Level of Care (ALC) patients. Nearly half (45.7%) were on at least one Beers Criteria drug. Many of these were unnecessary, and removing them improved their alertness and mobility.
The Centers for Medicare & Medicaid Services (CMS) now uses the Beers Criteria to measure quality in nursing homes and Medicare Part D plans. That means if a facility is prescribing too many flagged drugs, it could lose funding. That’s powerful - but it also creates pressure. Some doctors feel forced to avoid a drug even when it might help a patient. That’s where things get tricky.
It’s Not About Rules - It’s About Judgment
The American Geriatrics Society is very clear: the Beers Criteria are not meant to be used as a punishment tool. They’re not a checklist to cross off. They’re a conversation starter.For example, an antipsychotic might be prescribed for severe aggression in someone with advanced dementia. In most cases, it’s inappropriate. But if the person is hurting themselves or others, and every other option has failed, the risk-benefit balance changes. That’s where the doctor, the patient, and the family need to talk - not just check a box.
Pharmacist Christine Holman, who’s worked in VA hospitals for over a decade, puts it simply: “The Beers Criteria are a warning light, not a red stop sign.”
What works in one person might not work in another. A drug that causes dizziness in a healthy 75-year-old might be the only thing keeping a frail 88-year-old from falling. The goal isn’t to eliminate all risk - it’s to reduce the most dangerous risks without ignoring individual needs.
What Can You Do?
If you or someone you care for is over 65 and taking multiple medications, here’s what to do:- Ask for a medication review - Request a full list of all prescriptions, over-the-counter drugs, and supplements. Bring it to your doctor or pharmacist. Ask: “Are any of these on the Beers Criteria list?”
- Ask about alternatives - For example, instead of a benzodiazepine for anxiety, could cognitive behavioral therapy or low-dose SSRIs be safer? Instead of NSAIDs for joint pain, could physical therapy or acetaminophen work?
- Check for drug interactions - Many seniors take a mix of prescriptions and OTC meds. Even something as simple as antihistamines in cold medicine can interact dangerously with blood pressure pills.
- Use the free tools - The American Geriatrics Society offers a free mobile app and printable pocket card at GeriatricsCareOnline.org. There’s also a simplified version for families at healthinaging.org.
- Don’t stop meds on your own - If a drug is flagged, don’t quit it suddenly. Work with your provider to taper safely. Some drugs cause serious withdrawal if stopped abruptly.
What About Other Tools Like STOPP-START?
You might hear about STOPP-START - another set of guidelines for older adults. The difference? STOPP-START looks at both inappropriate drugs (STOPP) and drugs that are missing (START). So if an older adult with heart failure isn’t on a beta-blocker, START would flag that as a gap.The Beers Criteria don’t cover what’s missing. They only focus on what’s dangerous. That makes them narrower - but also easier to use in busy clinics. Many hospitals use both together: Beers to cut out bad drugs, STOPP-START to make sure good ones aren’t left out.
The Bottom Line
The Beers Criteria aren’t perfect. They can’t account for every individual’s story. But they’re the most widely used, evidence-based tool we have to protect older adults from harmful medications. They’ve helped reduce inappropriate prescribing in nursing homes by up to 30% in some studies. They’ve saved lives. They’ve prevented hospital stays. And they’ve started a much-needed conversation about what “safe prescribing” really means for aging bodies.The goal isn’t to stop all medication. It’s to make sure every pill has a reason - and that the reason is stronger than the risk.
Are all drugs on the Beers Criteria list completely banned for older adults?
No. The Beers Criteria are not absolute bans. They’re red flags. Some medications on the list may still be appropriate for certain individuals - for example, if no safer alternative exists or if the patient has a specific condition where the benefit outweighs the risk. The key is that these decisions should be made intentionally, with full understanding of the risks, and never just because it’s the easiest option.
Can I use the Beers Criteria to stop my own medications?
Never stop a prescribed medication on your own, even if it’s on the Beers list. Some drugs, like certain antidepressants or blood pressure medications, can cause serious withdrawal symptoms or rebound effects if stopped suddenly. Always talk to your doctor or pharmacist first. They can help you taper safely or find a better alternative.
Why are benzodiazepines on the Beers Criteria list?
Benzodiazepines - like lorazepam, diazepam, and alprazolam - increase the risk of falls, confusion, memory problems, and even car accidents in older adults. They’re also highly addictive and lose effectiveness over time. Studies show they don’t work better than non-drug options like sleep hygiene or cognitive behavioral therapy for insomnia. Even short-term use can be risky, which is why they’re flagged for most seniors.
Do the Beers Criteria apply to people under 65?
The Beers Criteria are specifically designed for adults aged 65 and older, based on age-related changes in how the body processes drugs. While some younger people with kidney disease, frailty, or multiple chronic conditions might benefit from similar caution, the list isn’t validated for use under 65. Other tools exist for younger populations, but Beers is targeted to the aging population.
How often are the Beers Criteria updated?
The American Geriatrics Society updates the Beers Criteria every three to five years, based on new research. The most recent version was published in 2023. The update process involves reviewing over 1,500 scientific studies and using a consensus method with a panel of geriatric experts, pharmacists, and clinicians to ensure the recommendations reflect the latest evidence.
Is the Beers Criteria used in Australia?
Yes. While Australia has its own guidelines - like the STOPP/START criteria and the Australian Medicines Handbook’s recommendations for older adults - the Beers Criteria are widely referenced by Australian geriatricians, pharmacists, and researchers. Many Australian hospitals and aged care facilities use Beers as a reference point, especially in settings with international staff or research ties. It’s not officially mandated like in the U.S., but it’s respected and used in clinical practice.
Next Steps for Families and Caregivers
If you’re helping an older adult manage their medications, start with this: write down every pill, patch, spray, and supplement they take - including aspirin, herbal teas, and vitamins. Bring that list to their next appointment. Ask: “Which of these are on the Beers list? Which ones are we still using for a good reason?”Don’t assume the doctor knows everything. Many prescribers aren’t geriatric specialists. But with the right questions, you can help turn a routine visit into a safety check.
The Beers Criteria aren’t about taking away meds. They’re about making sure every dose makes sense - and that no one is left vulnerable because a prescription was never questioned.



Just had a 79-year-old uncle on five Beers-listed meds-diazepam, ibuprofen, diphenhydramine, oxybutynin, and a PPI. Took him off three in three weeks. His balance improved, his memory cleared up, and he started cooking again. This list isn’t just theory-it’s life-changing if you actually use it.