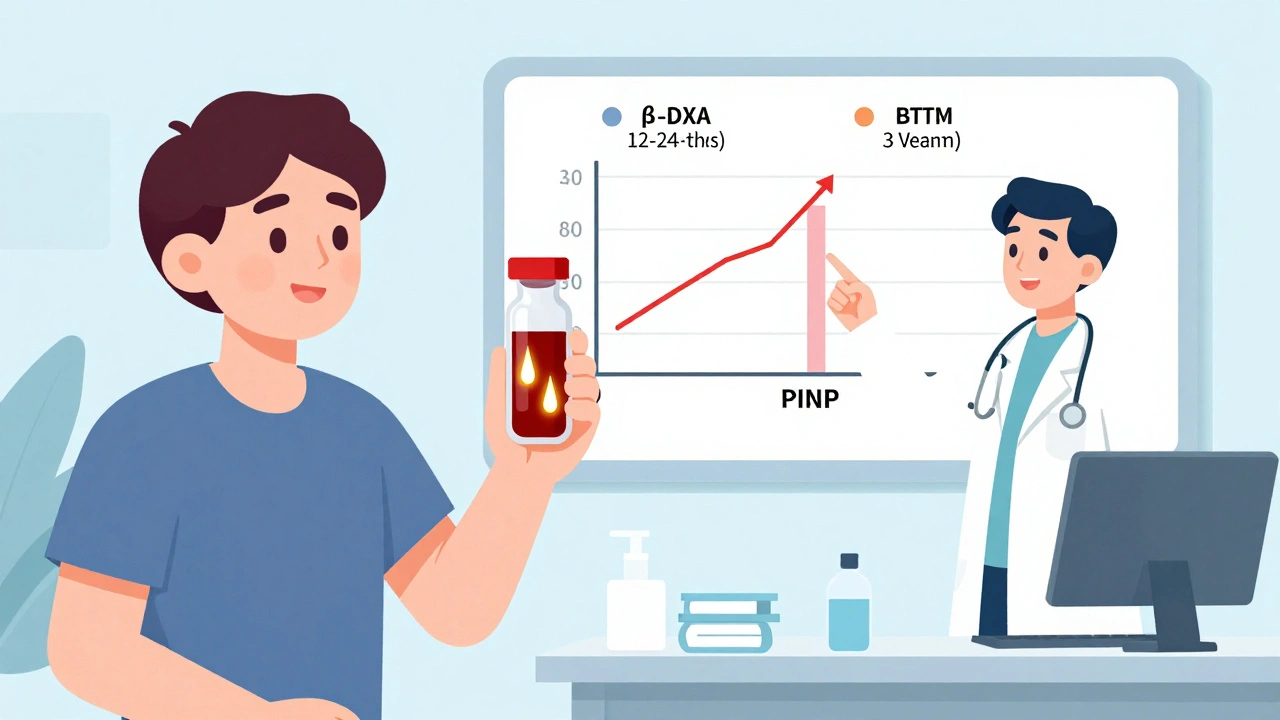
When you’re on medication for osteoporosis, waiting a year or two to see if it’s working can feel like guessing in the dark. Bone density scans (DXA) are the gold standard, but they don’t show results until 12 to 24 months after you start treatment. What if you could know sooner-within weeks-whether your therapy is actually working? That’s where bone turnover markers come in.
What Are Bone Turnover Markers?
Bone is always changing. Old bone breaks down, new bone forms. This process is called remodeling. Bone turnover markers (BTMs) are tiny proteins and fragments released into your blood or urine when bone is being broken down or built up. Think of them as signals from your skeleton telling you what’s happening inside.
There are two main types:
- Formation markers: Show new bone being made. The most reliable is PINP (procollagen type I N propeptide).
- Resorption markers: Show old bone being broken down. The gold standard here is β-CTX-I (beta C-terminal telopeptide of type I collagen).
These aren’t just lab curiosities. They’re now the recommended reference markers by the International Osteoporosis Foundation and European Calcified Tissue Society, based on years of research and standardized testing protocols.
Why Use Them Instead of Just a DXA Scan?
DXA scans measure bone density, but they’re slow. Even with effective treatment, it takes 1-2 years before you see a clear improvement on the scan. That’s a long time to wonder if your pills are doing anything.
Bone turnover markers change much faster. Within 3 to 6 weeks of starting an osteoporosis drug-whether it’s a bisphosphonate like alendronate or an anabolic agent like teriparatide-you’ll see measurable shifts in PINP or β-CTX-I levels.
For example:
- If you’re on an anti-resorptive drug (like a bisphosphonate), β-CTX-I should drop by more than 30% within 3-6 months.
- If you’re on teriparatide (which builds bone), PINP should spike by 70-100% within the same timeframe.
This early feedback is powerful. It tells you whether your body is responding-or whether you’re not taking your meds, your dose is wrong, or something else is interfering.
How Accurate Are They?
Not perfect-but reliable when done right. The precision of these tests is well-documented:
- PINP has an intra-assay variation of just 5.8% and inter-assay variation of 12.1%.
- β-CTX-I is even tighter: 3.5% intra-assay and 9.2% inter-assay.
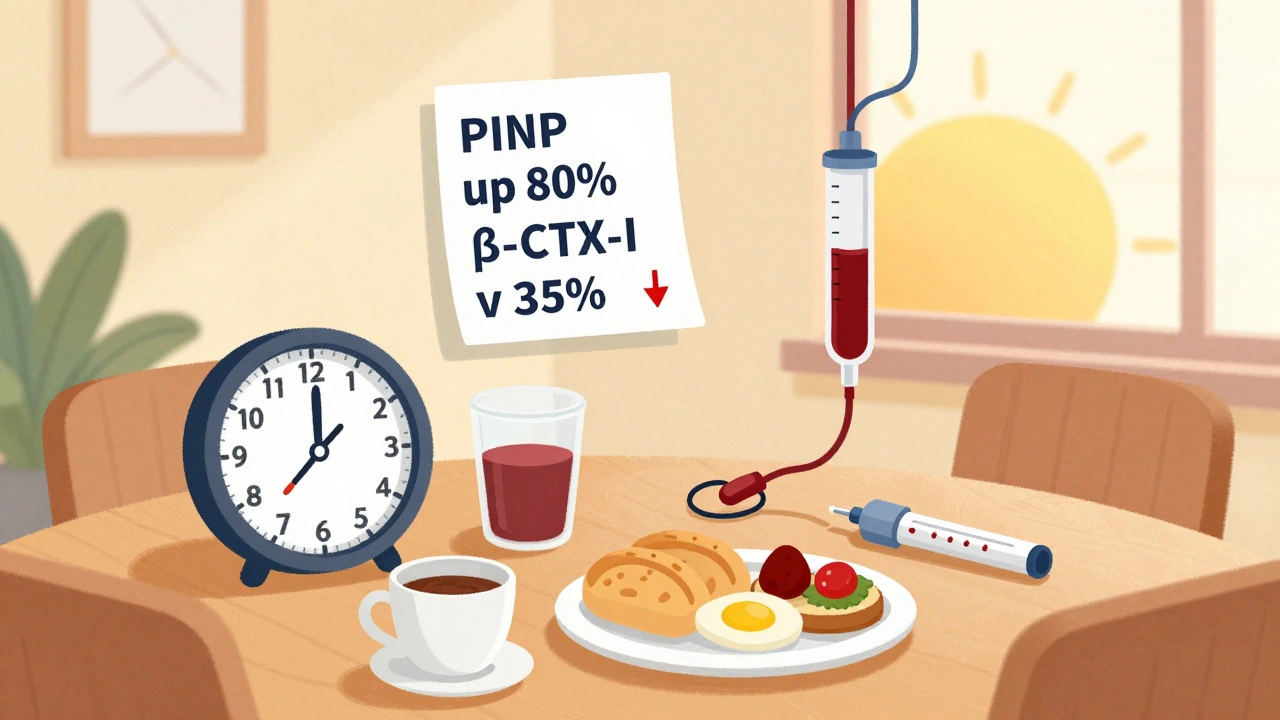
But accuracy depends heavily on how the sample is handled. For β-CTX-I, you must:
- Fast overnight (no food or drink except water)
- Have blood drawn between 8 and 10 a.m.
- Avoid eating or drinking anything but water for at least 2 hours before the test
Why? Bone resorption follows a daily rhythm. CTX levels can swing up to 40% between morning and evening. A sample taken after lunch could look like treatment isn’t working-when it’s just timing.
PINP is less affected by meals and time of day, but still best collected in the morning for consistency.
The smallest change that actually means something? A 20% drop for PINP and 25% drop for β-CTX-I. Anything less might just be normal variation.
Who Benefits Most From BTM Testing?
Bone turnover markers aren’t for everyone-but they’re game-changers for certain groups:
- Newly diagnosed patients: Starting treatment? Get a baseline BTM before you begin. Then retest at 3 months. That’s your first real check-in.
- Patients not responding: If your bone density hasn’t improved after a year, BTMs can tell you why. Are you non-adherent? Is your drug not working? Is there another condition interfering?
- People with kidney disease: Standard markers like PINP and β-CTX-I can be skewed by reduced kidney function. In these cases, bone alkaline phosphatase (BALP) or TRACP5b are better alternatives.
- Those on anabolic therapy: Teriparatide and romosozumab cause rapid bone formation. PINP is the best way to confirm the drug is triggering the intended response.
One study (the TRIO trial) showed patients who hit a >30% drop in β-CTX-I at 3 months had a 1.6% lower fracture risk after 22 weeks compared to those who didn’t respond. That’s not just a lab result-it’s a real-world reduction in broken bones.
Limitations and Misconceptions
Bone turnover markers aren’t a replacement for DXA scans. They don’t tell you how dense your bones are. They tell you how active your bone remodeling is.
They also have biological variability. Your levels can jump around 20-60% due to factors like:
- Menstrual cycle (in premenopausal women)
- Recent fractures or surgery
- Severe illness or prolonged bed rest
- High vitamin D or calcium intake
That’s why you need a baseline and repeat testing under the same conditions. One test alone means nothing.
Also, not all labs do these tests the same way. Only about 65% of U.S. labs follow the recommended IFCC protocols. Ask your doctor if the lab uses standardized assays for PINP and β-CTX-I.
What Does the Science Say?
The evidence is strong and growing. The 2023 consensus from the International Osteoporosis Foundation, European Society for Clinical and Economic Aspects of Osteoporosis, and International Federation of Clinical Chemistry and Laboratory Medicine clearly states: “Serum PINP and plasma β-CTX-I are the reference bone turnover markers for clinical use.”
Experts like Professor Eugene McCloskey and Professor Cyrus Cooper say these markers are “invaluable tools” for monitoring adherence and predicting response. A 2022 study in Orthopedic Reviews found BTM monitoring could identify non-adherent patients with 85% accuracy.
Health economists estimate that using BTMs to catch non-responders early can save $1,200-$1,800 per patient per year by avoiding unnecessary medication costs.
How to Get Tested
In the U.S., Medicare covers PINP (CPT code 83970) and β-CTX-I (CPT code 83935) for osteoporosis monitoring. Reimbursement is around $28-$33 per test. In Australia and Europe, adoption is higher-up to 60% of clinics use them routinely.
Here’s the practical flow:
- Get a baseline BTM test before starting treatment.
- Take your medication as prescribed-no skipping doses.
- Return for a repeat test at exactly 3 months.
- Compare results to baseline using the least significant change (LSC): >30% drop for β-CTX-I, >35% drop for PINP = good response.
- Continue treatment if responding. If not, talk to your doctor about switching or investigating adherence.
- Get a DXA scan at 12-24 months for final confirmation.
It’s simple. But it requires coordination between you, your doctor, and the lab. Don’t just show up for a blood test without fasting or at 3 p.m.-it’ll give you misleading results.
The Future of Bone Health Monitoring
Point-of-care BTM tests are in development. Imagine getting your PINP result during your doctor’s visit-no waiting days for lab results.
Research is also expanding reference ranges beyond Caucasian populations. Studies show Asian populations have 15-20% lower baseline β-CTX-I levels, and African populations have higher PINP. Current reference ranges may not fit everyone.
The American Association of Clinical Endocrinologists is expected to update its guidelines in 2024 to include formal BTM recommendations. That will push adoption even further.
For now, the message is clear: if you’re being treated for osteoporosis, ask about bone turnover markers. They’re not magic-but they’re the fastest, most direct way to know if your treatment is working before it’s too late.
Are bone turnover markers better than DXA scans for monitoring osteoporosis?
No, they’re not better-they’re complementary. DXA scans measure bone density and are the gold standard for diagnosis and long-term monitoring. Bone turnover markers show how quickly your bones are remodeling and give early feedback on treatment response. Use BTMs at 3 months to see if your drug is working; use DXA at 12-24 months to confirm bone density improved.
How often should bone turnover markers be tested?
Test once before starting treatment, then again at 3 months. After that, repeat every 6-12 months only if your doctor suspects non-response or non-adherence. Routine annual testing isn’t needed unless your situation changes.
Do I need to fast before a bone turnover marker test?
Yes-for β-CTX-I, you must fast overnight and have blood drawn between 8-10 a.m. Food and time of day can cause major fluctuations. PINP is less sensitive, but for consistency, it’s best to fast and test in the morning for both markers.
Can bone turnover markers predict fracture risk?
They’re not direct predictors like DXA, but they’re strong indicators of treatment effectiveness. Patients who show a >30% drop in β-CTX-I within 3 months have a significantly lower fracture risk over the next year. High turnover rates, even with normal bone density, can signal higher fracture risk.
Why aren’t bone turnover markers used more often?
Mainly because of preanalytical challenges-timing, fasting, lab standardization-and lack of clinician awareness. Many doctors still rely only on DXA scans. But adoption is growing, especially in Europe and among endocrinologists. Insurance coverage in the U.S. has improved since 2020, and guidelines are updating to reflect their value.
What if my bone turnover markers don’t change after 3 months?
That’s a red flag. It could mean you’re not taking your medication, your dose is too low, or another condition (like vitamin D deficiency or kidney disease) is interfering. Talk to your doctor. You may need to switch drugs, adjust your dose, or investigate underlying issues. Non-response is a signal to act-not to wait another year.


Okay so i was reading this and honestly? Bone turnover markers are like the VIP pass for osteoporosis treatment. I mean, why wait 2 years for a DXA when you can get a blood test and know in 3 weeks if your meds are even doing anything? My endo started doing this after my last fracture and honestly? Game changer. PINP went up 80% in 12 weeks on teriparatide. I felt like my bones were yelling at me to keep going.