Sulfonylurea Safety Risk Calculator
Compare Your Risk
Enter your health factors to see which sulfonylurea has the lowest hypoglycemia risk for you.
Your Safety Recommendation
Risk Comparison
Based on your inputs, glipizide has the lowest hypoglycemia risk. Glyburide is associated with significantly higher risk, especially for patients over 65, with kidney issues, or irregular eating patterns. Consider discussing this risk profile with your doctor.
Recommendation
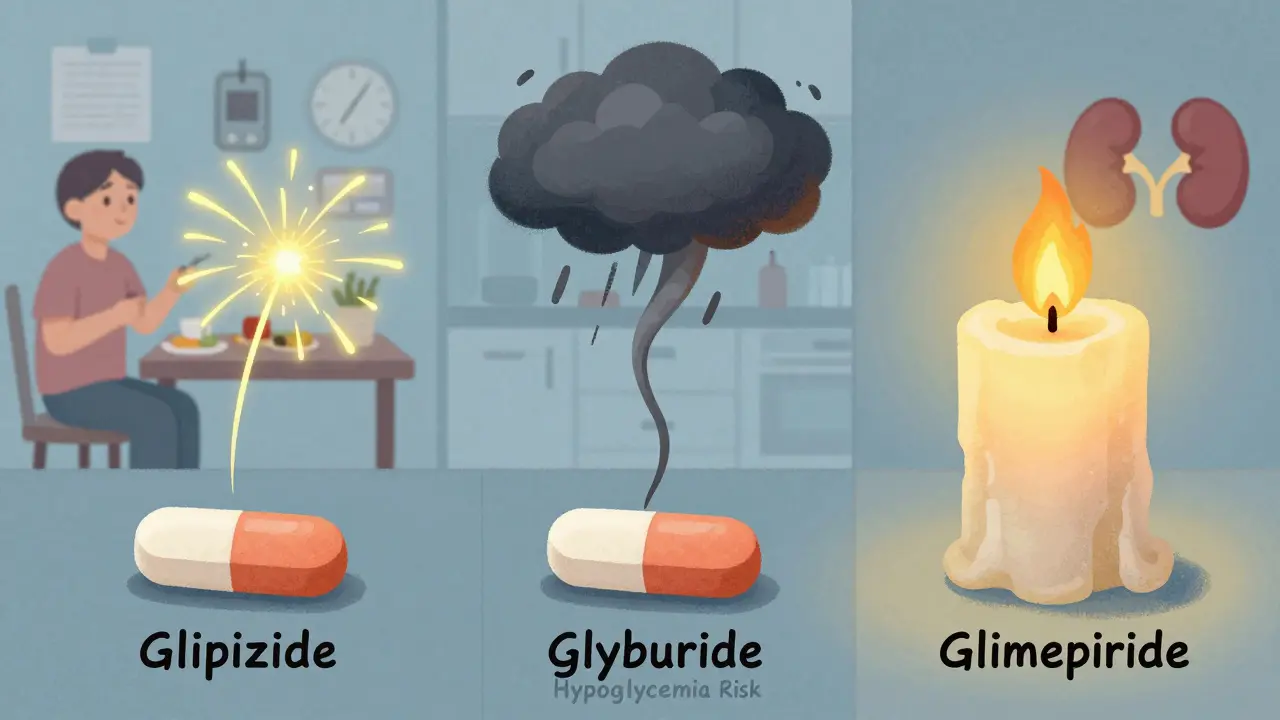
When you’re managing type 2 diabetes, picking the right medication isn’t just about lowering blood sugar-it’s about staying safe. Among older drugs still widely used, sulfonylureas deliver strong results at low cost. But not all sulfonylureas are the same. Some put you at much higher risk of dangerous low blood sugar episodes, especially if you’re older, have kidney issues, or skip meals. The difference between choosing glipizide versus glyburide could mean the difference between a manageable side effect and an emergency room visit.
Why Sulfonylureas Still Matter
Sulfonylureas have been around since the 1950s, and they’re still prescribed to millions of people with type 2 diabetes. Why? Because they work. They force the pancreas to release more insulin, which pulls glucose out of the blood. In clinical trials, they typically lower HbA1c by 1.5% to 2.0%. That’s as good as many newer drugs. But here’s the catch: they’re cheap. Generic glipizide costs about $4 a month. Compare that to semaglutide (Ozempic), which runs over $500 a month. For people on Medicare, Medicaid, or without insurance, sulfonylureas are often the only realistic option. In low- and middle-income countries, they’re the backbone of diabetes care. But cost shouldn’t blind you to risk.The Hypoglycemia Problem: Not All Sulfonylureas Are Created Equal
The biggest danger with sulfonylureas is hypoglycemia-when your blood sugar drops too low. Symptoms include shaking, sweating, confusion, dizziness, and in severe cases, seizures or coma. And the risk isn’t the same across all drugs in this class. Glyburide (also called glibenclamide) is the worst offender. Studies show it causes nearly three times more severe hypoglycemia than glipizide. Why? Because it sticks around too long. Glyburide has a half-life of about 10 hours, and its metabolites stay active for up to 24 hours. That means even if you eat late or skip a meal, the drug is still forcing your pancreas to pump out insulin. Your blood sugar crashes. And because it’s long-acting, recovery takes longer. Glipizide, on the other hand, works fast and leaves fast. Its half-life is only 2 to 4 hours. It’s designed to match meal times. You take it 30 minutes before breakfast or dinner, it helps lower your spike, then it’s mostly gone by the next meal. That’s why a 2019 analysis in the American Journal of Managed Care found glipizide caused just 4.2 hypoglycemia episodes per 1,000 patient-years-compared to 12.1 for glyburide. Glimepiride sits in the middle. It’s longer-acting than glipizide but not as risky as glyburide. Still, studies show it causes nearly twice as many low blood sugar events as glipizide.What the Experts Say
The American Geriatrics Society’s 2023 Beers Criteria-widely followed by doctors treating older adults-explicitly says: avoid glyburide in patients 65 and older. Why? Because older adults are more sensitive to insulin, often have kidney decline, and may forget to eat. Glyburide’s long action turns a minor slip-up into a medical crisis. Dr. Robert A. Vigersky, a leading endocrinologist, put it bluntly: “The choice between sulfonylureas isn’t whether to use them, but which one to use based on the patient’s hypoglycemia risk profile.” The American Diabetes Association’s 2024 Standards of Care now recommend preferring short-acting sulfonylureas like glipizide over long-acting ones like glyburide or glimepiride-especially for elderly patients or those with irregular eating habits. Even the FDA and European Medicines Agency have taken action. Since 2017, sulfonylurea labels must carry stronger warnings about hypoglycemia. In Europe, glyburide is restricted for patients over 75.Real People, Real Consequences
Behind the numbers are real stories. On the American Diabetes Association’s online forum, a 2023 thread titled “Switching from glyburide to glipizide” had 87 responses. Sixty-three people-72%-reported fewer low blood sugar episodes after switching. One user wrote: “I was having 2-3 severe lows every month on glyburide. Since switching to glipizide, I’ve had zero.” On Reddit, a thread about glyburide side effects had 68 responses. Forty-one of them-60%-described ER visits due to low blood sugar. One 72-year-old man said: “I spent three days in the hospital after my kidney function dropped. My endocrinologist admitted he never should’ve prescribed glyburide.” The FDA’s adverse event database confirms this. From 2018 to 2022, glyburide accounted for 68% of all sulfonylurea-related hypoglycemia reports-even though it was only prescribed in about 36% of cases.
Who Should Avoid Glyburide and Glimepiride?
These drugs aren’t just risky for the elderly. They’re dangerous for anyone with:- Chronic kidney disease (eGFR below 60 mL/min/1.73m²)
- Irregular meal schedules
- History of hypoglycemia
- Alcohol use
- Older age (65+)
What About Gliclazide?
Gliclazide isn’t available in the U.S., but it’s widely used in Europe, Canada, and Australia. It’s considered “pancreas-specific,” meaning it targets insulin release more precisely and causes less hypoglycemia than glyburide. A 2017 study found its hypoglycemia rate was similar to glipizide-around 3.8 episodes per 1,000 patient-years. It’s also been linked to fewer cardiovascular events in some studies. If you’re outside the U.S., ask your doctor if gliclazide is an option.New Options Are Coming
In 2023, the FDA approved an extended-release version of glipizide called Glucotrol XL. Early data shows it lowers hypoglycemia risk by 32% compared to the regular version. Why? Because it releases the drug slowly, avoiding the sharp insulin spikes that cause lows. This could make glipizide even safer. Meanwhile, a large ongoing trial called SURE-DM3 is comparing glipizide and gliclazide in over 1,200 elderly patients. Results are expected in late 2025. If the findings hold, we may see stronger global recommendations for these safer options.How to Use Sulfonylureas Safely
If you’re on a sulfonylurea, here’s what you need to do:- Know which one you’re on. If it’s glyburide, talk to your doctor about switching to glipizide.
- Start low. Always begin with the smallest dose. For glipizide, that’s 2.5 mg. For glyburide, it’s 1.25 mg.
- Take it before meals. Glipizide should be taken 30 minutes before breakfast or dinner. Don’t skip meals after taking it.
- Learn the 15-15 rule. If you feel shaky or sweaty, check your blood sugar. If it’s below 70 mg/dL, eat 15 grams of fast-acting carbs (like 4 oz of juice or 3-4 glucose tablets). Wait 15 minutes. Check again. Repeat if needed.
- Get kidney tests. Have your eGFR checked at least once a year. If it drops, your dose may need adjusting-or you may need a different drug.
- Warn your family. Hypoglycemia can make you confused or unconscious. Make sure someone close to you knows how to help.
Is There a Better Alternative?
Yes. Newer drugs like SGLT2 inhibitors (empagliflozin, dapagliflozin) and GLP-1 receptor agonists (semaglutide, liraglutide) have far lower hypoglycemia risk. They also protect the heart and kidneys. But they’re expensive. For many people, especially on Medicare, sulfonylureas remain the only affordable choice. The key isn’t to avoid sulfonylureas entirely. It’s to choose the right one-and use it smartly. Glipizide, taken correctly, can be a safe, effective tool. Glyburide? It’s a relic that belongs in the past.What to Ask Your Doctor
If you’re on a sulfonylurea, ask:- “Which sulfonylurea am I taking-glipizide, glyburide, or glimepiride?”
- “Is this the safest option for me, given my age, kidney function, and eating habits?”
- “Would switching to glipizide reduce my risk of low blood sugar?”
- “Should I get my kidney function checked?”
- “Do I need a glucagon kit or a medical alert bracelet?”
Diabetes management has changed. The goal isn’t just to lower blood sugar-it’s to do it without putting your life at risk. Choosing the right sulfonylurea isn’t a small detail. It’s a life-saving decision.


My dad switched from glyburide to glipizide last year after three ER trips. He’s 78, has stage 2 kidney disease, and used to wake up drenched in sweat at 3 a.m. Now? Zero lows. He even forgot his glucose tabs once and just ate a banana. No drama. Seriously, if you’re on glyburide and over 65, talk to your doc today.