When you’re on warfarin, the last thing you want is a surprise blood clot-or worse, a bleed. And for years, the advice was simple: avoid spinach, kale, and broccoli. But that advice is wrong. Today, doctors and dietitians agree: it’s not about cutting out green leafy vegetables. It’s about keeping your intake consistent.
Why Vitamin K Matters with Warfarin
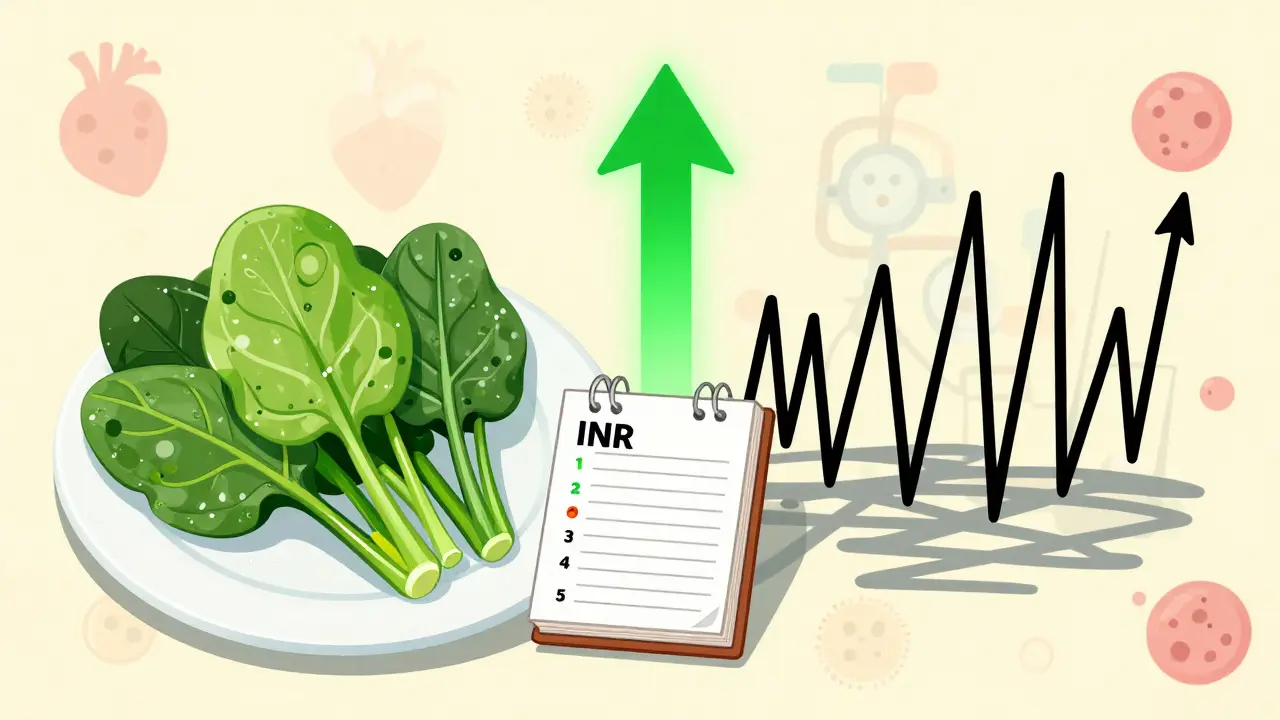
Warfarin works by blocking vitamin K’s role in blood clotting. Vitamin K is what your body uses to make clotting factors-proteins that stop you from bleeding out after an injury. Warfarin slows this process down, thinning your blood to prevent dangerous clots. But if your vitamin K intake jumps up or down, your blood’s clotting ability shifts too. That’s measured by your INR (International Normalized Ratio). A normal therapeutic range is usually between 2.0 and 3.0. Go outside that, and your risk goes up: low INR means clots; high INR means bleeding.The Real Culprit: Inconsistency, Not Vegetables
You don’t need to stop eating kale. You just need to eat about the same amount every day. A 2024 study from the National Institutes of Health found that patients taking warfarin could safely eat up to 100 grams of spinach daily-about one large handful-if they ate it every single day. The same study showed that when people changed their intake suddenly-say, from one cup of spinach a week to five cups in a week-their INR dropped sharply within days. Here’s the data on vitamin K in common greens (per cooked cup):| Vegetable | Vitamin K (mcg) |
|---|---|
| Spinach | 889 |
| Kale | 547 |
| Collard greens | 772 |
| Swiss chard | 573 |
| Broccoli | 220 |
| Cabbage | 108 |
The recommended daily intake for adults? 90-120 mcg. That means a single cup of cooked spinach has nearly 10 times your daily need. But if you eat one cup every day, your body adjusts. Warfarin dosing can be fine-tuned to match that level. The problem isn’t the food. It’s the chaos.
What Happens When You Change Your Diet?
If you suddenly start eating more vitamin K-say, you add a big spinach salad every day-you’re giving your body more of the thing warfarin is trying to block. Your INR will drop. That means your blood clots faster. You’re at higher risk for stroke or pulmonary embolism. If you suddenly eat less-maybe you went on a juice cleanse and skipped your kale smoothie-your INR will rise. That means your blood thins too much. You could bruise easily, bleed for longer, or even have internal bleeding. The University of Iowa Hospitals & Clinics warns that a 50% increase or decrease in daily vitamin K can shift your INR by 0.5 to 1.0 points in just 3-5 days. That’s enough to push you out of your safe range.
What Can You Eat Without Worrying?
You don’t have to give up vegetables. You just need to pick the low-vitamin K ones for days you’re not eating your usual greens. The NHS gives clear, practical examples:- Lettuce - ½ cup (80g)
- Carrots - 3 dessert spoons
- Cauliflower - 8 florets
- Courgette (zucchini) - ½ a large one
- Mushrooms - 3-4 dessert spoons
These can be eaten freely, without tracking. They contain less than 20 mcg of vitamin K per serving. That’s safe even if you’re not eating your regular spinach or kale that day.
Warfarin vs. Newer Blood Thinners
You might be wondering: why not just switch to a newer drug? Drugs like apixaban (Eliquis), rivaroxaban (Xarelto), and dabigatran (Pradaxa) don’t interact with vitamin K at all. No diet restrictions. No INR checks. That’s why 68% of patients who switched cited diet as their main reason. But warfarin still has its place. For people with mechanical heart valves-especially in the mitral position-DOACs (direct oral anticoagulants) aren’t approved. Warfarin is the only option. It’s also preferred for those with severe kidney disease (eGFR under 15), and for people with antiphospholipid syndrome. And cost? Warfarin costs $4-$10 a month. The newer drugs? $500-$600. For many, that’s not a choice-it’s a necessity.What to Avoid (Besides Inconsistent Eating)
It’s not just vegetables. Some supplements and foods can mess with warfarin too:- St. John’s Wort - can lower INR
- Danshen (Chinese herb) - increases bleeding risk
- Ginkgo Biloba - thins blood further
- Grapefruit juice - interferes with how warfarin is broken down
- Cod liver oil - high in vitamin A and D, which can affect clotting
- Glucosamine - may raise INR in some people
And if you’re sick-diarrhea, fever, stomach bugs-your body absorbs vitamin K differently. That’s when INR can swing unexpectedly. If you’re unwell for more than a few days, call your doctor. Don’t wait for your next check-up.

How to Stay on Track
The goal isn’t perfection. It’s predictability.- Choose one or two high-vitamin K greens you like (spinach, kale, collards) and eat the same portion every day.
- Use a food scale for the first few weeks. 100g of spinach is about one packed cup. Stick to that.
- On days you skip your usual green, fill in with low-vitamin K veggies like carrots, mushrooms, or lettuce.
- Keep a simple log: what you ate, when, and your INR reading. You don’t need an app-just a notebook.
- Get your INR checked every 2-4 weeks when stable. More often if you change your diet or feel unwell.
Researchers at the University of Iowa are now testing digital tools that help patients track vitamin K intake. Early results show these tools reduce INR variability by 27% compared to standard advice. That’s huge.
What Experts Say
Joan Salge Blake, a registered dietitian at Boston University, put it plainly: “The key to preventing fluctuations in warfarin’s effectiveness is to maintain a consistent intake of vitamin K.” The Mayo Clinic says: “Do not change the amounts of vitamin K-rich foods or drinks you have from day to day or week to week.” The American College of Chest Physicians says it even more clearly in their 2021 guidelines: “We suggest that patients receiving vitamin K antagonists maintain a consistent intake of vitamin K rather than avoiding vitamin K-rich foods.” There’s no debate among medical authorities. Avoidance doesn’t work. Consistency does.Bottom Line
You can still enjoy your greens. You just need to be steady. Eat your spinach. Eat your kale. But eat the same amount every day. That’s how you keep your INR stable, your blood clotting right, and your life free from unnecessary hospital trips.Warfarin isn’t going away. And neither are leafy greens. The smart move isn’t to choose between them. It’s to learn how to live with both.
Can I eat spinach if I’m on warfarin?
Yes, you can eat spinach while on warfarin. The key is consistency. A 2024 NIH study confirmed that eating up to 100 grams (about one large cup) of spinach daily is safe if you eat the same amount every day. Sudden changes in intake-like going from once a week to daily-are what cause dangerous INR shifts.
What happens if I eat more kale one week than usual?
Eating more kale or other high-vitamin K greens can lower your INR, meaning your blood clots faster. This raises your risk of stroke or blood clots. A 50% increase in vitamin K intake can drop your INR by 0.5-1.0 points within 3-5 days. That’s enough to move you out of your safe range. If you eat more one week, expect to need a warfarin dose adjustment.
Are there vegetables I can eat without worrying?
Yes. Vegetables with low vitamin K content-like carrots (3 dessert spoons), lettuce (½ cup), cauliflower (8 florets), mushrooms (3-4 dessert spoons), and zucchini (½ large)-can be eaten freely without tracking. They contain less than 20 mcg of vitamin K per serving and won’t affect your INR.
Should I switch from warfarin to a newer blood thinner?
It depends. Newer drugs like Eliquis and Xarelto don’t interact with vitamin K, so no diet changes are needed. But warfarin is still the best option for people with mechanical heart valves, severe kidney disease, or antiphospholipid syndrome. Also, warfarin costs $4-$10 a month, while newer drugs cost $500-$600. Talk to your doctor about your medical needs and financial situation before switching.
What supplements should I avoid with warfarin?
Avoid St. John’s Wort, Danshen, Ginkgo Biloba, glucosamine, and cod liver oil. These can interfere with warfarin’s effect-either making it less effective or increasing bleeding risk. Grapefruit juice can also alter how your body breaks down warfarin. Always check with your doctor or pharmacist before taking any supplement.
How often should I get my INR checked?
When your dose is stable, most people check INR every 2-4 weeks. But if you change your diet, get sick, start a new medication, or notice unusual bruising or bleeding, check more often-weekly or even twice a week. Your doctor will adjust frequency based on your stability.
Is it okay to eat broccoli on warfarin?
Yes. Broccoli contains about 220 mcg of vitamin K per cooked cup-less than spinach or kale but still significant. If you eat broccoli regularly, keep the portion the same each day. If you usually eat ½ cup three times a week, stick to that. Don’t suddenly double it or skip it for weeks.
Can I drink green smoothies while on warfarin?
Yes, but be careful. A green smoothie with kale, spinach, and parsley can contain over 1,000 mcg of vitamin K-more than 10 times your daily need. If you drink them, make sure they’re consistent. Use the same ingredients and amounts every time. If you usually have one with ½ cup spinach, don’t switch to 2 cups without talking to your doctor.
If you’re on warfarin, your diet doesn’t need to be restrictive-it needs to be reliable. Eat your greens. Just eat the same amount, every day.


So let me get this straight: the government, Big Pharma, and your doctor are all in cahoots to keep you eating kale-so you’ll keep coming back for warfarin refills? But here’s the twist: they’ve been lying about vitamin K for decades! The real story? The FDA approved spinach as a ‘natural anticoagulant suppressant’ in 1987-secretly!-and now they want you to believe consistency is the answer? HA! I’ve been eating 3 pounds of raw kale daily for 11 years-my INR? Fluctuates like a stock market crash. Coincidence? I think not.