When women start thinking about hormone therapy after menopause, it’s not just about taking a pill. It’s about matching the right mix of hormones to your body, your history, and your goals. Many assume all hormone therapies are the same, but the truth is more complex. There are different combinations, delivery methods, and generic options - and choosing wrong can mean more side effects, or even serious risks.
Why Combinations Matter
Not every woman needs the same hormones. If you’ve had a hysterectomy, you only need estrogen. But if you still have your uterus, you must take progesterone (or a progestogen) along with estrogen. Why? Because estrogen alone makes the lining of your uterus grow. Left unchecked, that can lead to endometrial cancer. The NHS says this risk jumps 2 to 12 times higher without progestogen. That’s not a small detail - it’s a dealbreaker.That’s why there are two main types of combination therapy: sequential and continuous. Sequential means you take estrogen every day, and add progestogen for 10 to 14 days each month. It mimics your old cycle. You’ll still get monthly bleeding - which is fine if you’re in perimenopause and still having periods. Continuous combined means you take both hormones every single day. No breaks. This is for women who haven’t had a period for a full year. No monthly bleeding. That’s often the goal for postmenopausal women.
Generic Options You Can Actually Use
Most hormone prescriptions today are generic. They’re cheaper, just as effective, and widely available. Common generic estrogen options include:- Conjugated estrogens - 0.3mg, 0.45mg, or 0.625mg tablets
- Estradiol - 0.5mg or 1mg tablets
For progestogen, the most common generics are:
- Medroxyprogesterone acetate - 2.5mg, 5mg, or 10mg tablets
These are the backbone of HRT in the U.S. market. According to GoodRx data from October 2023, monthly costs range from $4 to $40, depending on your insurance and the dose. That’s a huge difference from branded versions that can cost over $100. Generic drugs aren’t second-rate - they’re chemically identical to the brand names. The FDA requires them to meet the same standards.
Delivery Methods: Patch, Gel, or Pill?
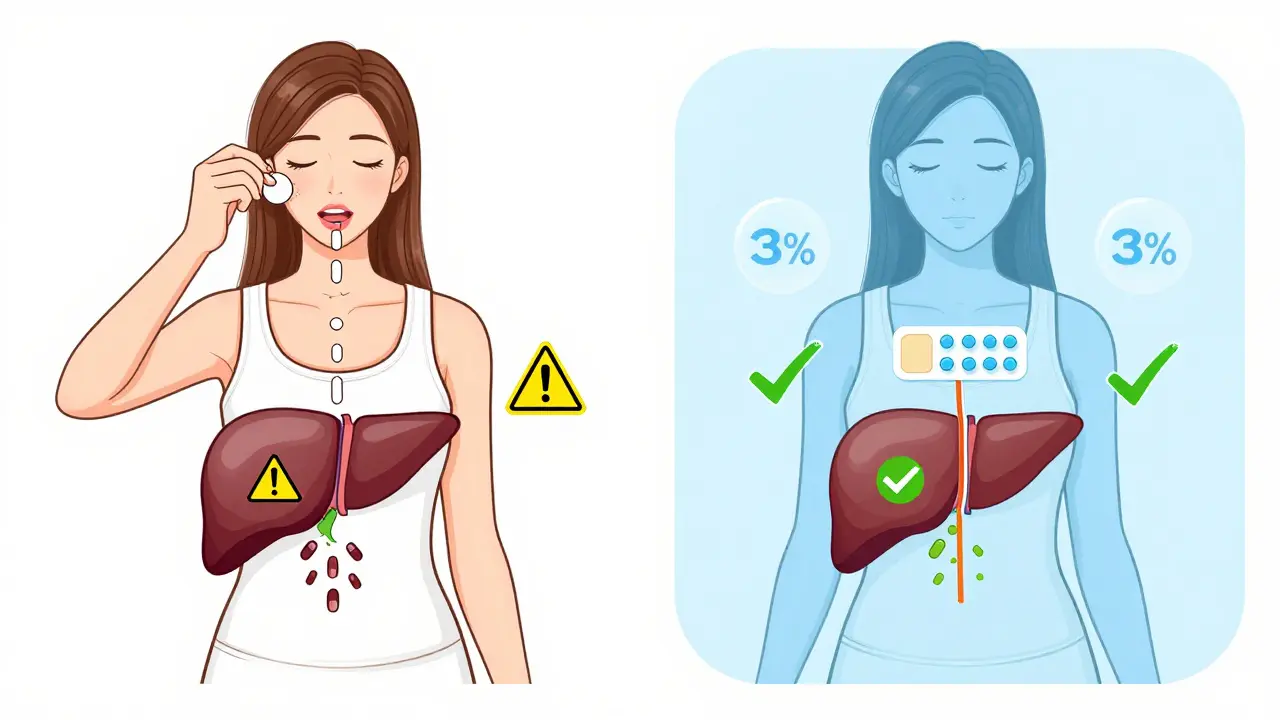
How you take your hormones matters just as much as which ones you take. Oral pills are the most common - but they’re not always the safest.When you swallow estrogen, it goes straight to your liver. That forces your liver to work harder, which can raise your risk of blood clots. NIH research shows oral HRT increases the chance of venous thromboembolism (VTE) by 2 to 3 times compared to skin-based methods. That’s why patches, gels, and sprays are becoming more popular. They deliver estrogen directly into your bloodstream, skipping the liver entirely.
Transdermal patches are replaced twice a week. Gels go on your arm or thigh every morning. Both have lower risks of clots and strokes. For women over 60 or with a history of heart issues, transdermal estrogen is often the only safe choice. The Women’s Health Initiative found oral estrogen increases stroke risk by 39% in women over 60. Patches? Not so much.
There’s also the Mirena IUD - a tiny device placed in the uterus that releases progestogen locally. It’s great for women who need progestogen but want to avoid pills altogether. It cuts uterine bleeding and protects against cancer without affecting your whole body.
Who Should Avoid HRT?
HRT isn’t for everyone. The American College of Obstetricians and Gynecologists (ACOG) says it’s only for managing symptoms - not for preventing heart disease, dementia, or osteoporosis. If you’re over 60, or more than 10 years past menopause, starting HRT now can do more harm than good. Dr. Gutierrez from Houston Methodist Hospital puts it bluntly: “Throw hormones at an older person with heart disease, and you’re asking for trouble.”Women with a history of breast cancer, blood clots, stroke, or liver disease should generally avoid systemic HRT. Even if you’re healthy, long-term use of combined therapy increases breast cancer risk. The Cleveland Clinic reports the risk rises by less than 1 in 1,000 per year - but after five years, it becomes measurable. That’s why experts recommend the lowest dose for the shortest time needed.
Progestogen Type: Synthetic vs. Natural
Not all progestogens are created equal. Most generic pills use medroxyprogesterone acetate - a synthetic version. But there’s another option: micronized progesterone. It’s derived from plants and matches your body’s natural progesterone exactly.Here’s the key difference: synthetic progestins raise breast cancer risk faster. According to the European Menopause and Andropause Society (EMAS), each year of synthetic progestin use increases risk by 2.7%. With micronized progesterone? Just 1.9%. That might not sound like much, but over five years, it adds up. If you’re planning long-term therapy, asking for micronized progesterone could make a real difference.
Unfortunately, micronized progesterone isn’t always covered by insurance. It’s often more expensive than medroxyprogesterone. But if you’re concerned about breast cancer risk - especially if you have a family history - it’s worth discussing.
What to Expect When You Start
Most women don’t feel better overnight. It takes 3 to 6 months to find the right dose and delivery method. During that time, you might get breakthrough bleeding - especially if you’re on sequential therapy. That’s normal. About 15-20% of women experience it in the first six months. But if it lasts longer than six months, or if bleeding becomes heavy or irregular, you need to see your doctor. It could mean the dose is wrong, or something else is going on.Also, how you apply the gel or patch matters. If you put gel on and then hug someone right away, they could absorb it through their skin. That’s why you need to wait 60 minutes before skin-to-skin contact. Patches need to stick well - if they peel, the dose drops. Always check the instructions. Small mistakes can make a big difference.
What’s New in 2026?
The field is evolving. In 2023, the FDA approved a new transdermal patch that combines estrogen and progesterone in one patch. Early data from the TWIRP study suggests it may carry a lower breast cancer risk than traditional oral combos. The North American Menopause Society now recommends annual reviews after the first 3-5 years of treatment. And research from the KEEPS study shows that starting transdermal estradiol within three years of menopause may actually protect your heart - without increasing artery plaque.Future options are coming too. TSECs (tissue-selective estrogen complexes) and SPRMs (selective progesterone receptor modulators) are in late-stage trials. These aim to give you symptom relief without triggering breast or uterine risks. They’re not on the market yet - but they’re the next wave.
Bottom Line
Hormone therapy isn’t a one-size-fits-all treatment. Your choice depends on:- Whether you still have your uterus
- Your age and how long it’s been since menopause
- Your personal and family health history
- Your tolerance for side effects
- And yes - your budget
Generic options are safe, effective, and affordable. Transdermal delivery is safer than pills for most women. Micronized progesterone beats synthetic if you’re worried about breast cancer. And always start low, go slow, and reassess every year. You’re not just treating hot flashes - you’re protecting your long-term health.



So let me get this straight - you’re telling me that if I don’t take progesterone with estrogen, my uterus is gonna turn into a cancer factory? And you call this medicine? This isn’t treatment, it’s hostage negotiation. The FDA approves this? I’d rather just duct tape my ovaries and call it a day.
Also, why is medroxyprogesterone acetate the default? Who’s利益着? Big Pharma? Because micronized progesterone costs 3x more and works better - but nope, let’s keep the synthetic crap on the shelf. It’s not science, it’s corporate theater.