DVT and Pulmonary Embolism Risk Assessment
Personal Risk Assessment
Answer a few questions about your health history and lifestyle to assess your risk of developing deep vein thrombosis (DVT) or pulmonary embolism (PE).
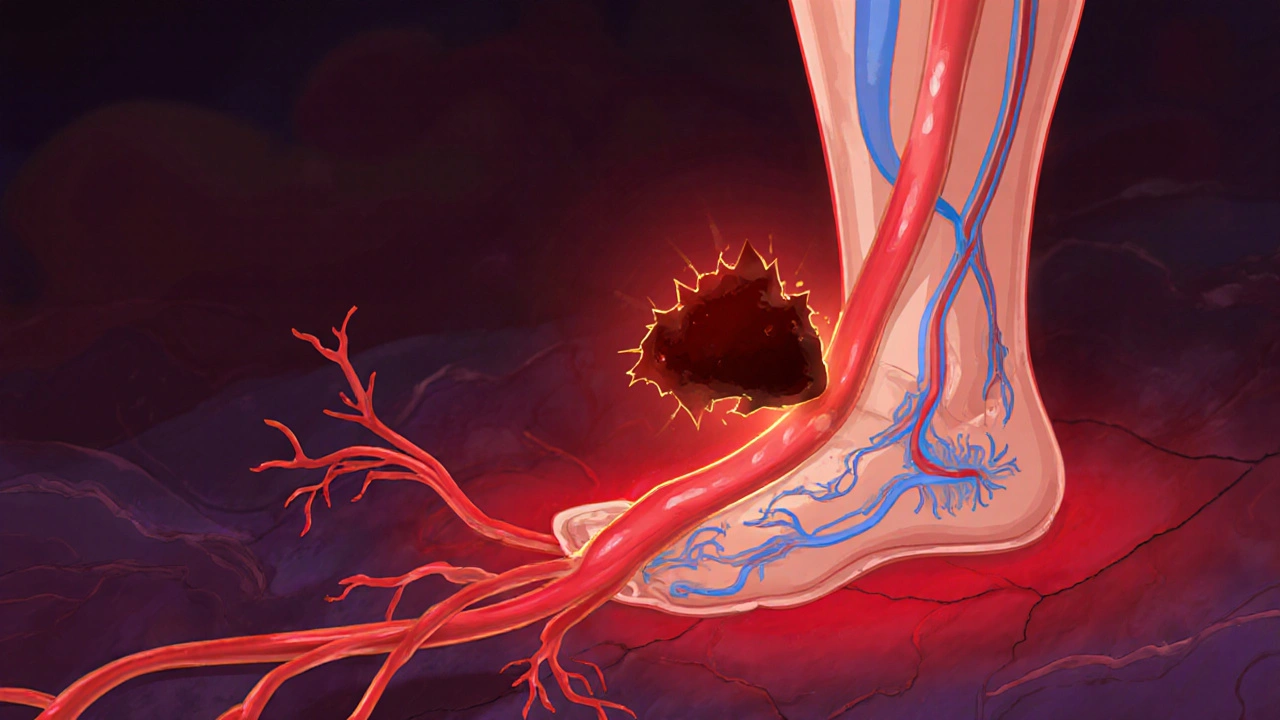
Deep vein thrombosis (DVT) is a blood clot that forms in the deep veins, most often in the legs. When you sit for hours on a plane, recover from surgery, or have a genetic clotting disorder, those veins can become sluggish and a clot can grow unnoticed.
Once a clot forms, it doesn’t always stay put. Pulmonary embolism (PE) occurs when part of that clot breaks free, travels through the bloodstream, and lodges in the pulmonary arteries of the lungs. The blockage can shrink lung tissue, raise heart pressure, and, in severe cases, be fatal.
Why DVT and PE Are Two Sides of the Same Coin
Both conditions share the same underlying problem: a blood clot forming in the venous system. The clot’s composition-fibrin, platelets, and red blood cells-is identical whether it stays in the leg or ends up in the lungs. The key difference is the clot’s location, which determines the symptoms you notice and the urgency of treatment.
Pathway From Leg to Lung
The journey begins in the deep veins of the calf or thigh. As blood pools, the clot’s surface becomes exposed to the bloodstream’s pressure gradient. A piece can detach-a process called embolization. That fragment travels up the inferior vena cava, passes through the right side of the heart, and finally enters the pulmonary artery. If the clot is large enough, it can block one or more branches, reducing oxygen exchange and causing chest pain, shortness of breath, or even collapse.
Major Risk Factors That Link DVT to PE
- Immobility - long flights, bed rest, or sedentary work stifle the calf muscle pump.
- Surgery or trauma - especially orthopedic or abdominal procedures that damage vessels.
- Genetic clotting disorders - e.g., Factor V Leiden mutation increases clotting propensity.
- Cancer - tumors release pro‑coagulant substances and many chemotherapies heighten risk.
- Hormone therapy - oral contraceptives or hormone replacement can tip the balance toward clot formation.
How Doctors Spot a Dangerous Clot
When you report leg swelling, pain, or a sudden gasp of breath, clinicians start with a physical exam and a few key tests. The D-dimer test measures fibrin degradation products; a high result suggests a clot is breaking down somewhere in the body. If the result is positive, imaging follows:
- Compression ultrasonography - the first‑line tool for visualizing a DVT in the leg.
- CT pulmonary angiography (CTA) - the gold standard for confirming a PE, showing the exact location of the blockage.
Both tests are quick, widely available, and give doctors the evidence they need to start treatment.
Treatment Strategies That Target Both DVT and PE
Once a clot is confirmed, the goal is twofold: stop the clot from growing and prevent new clots from forming. Anticoagulant therapy-usually a direct oral anticoagulant (DOAC) or heparin bridge-does exactly that. In high‑risk PE, physicians may also consider thrombolysis (clot‑busting drugs) or catheter‑directed clot removal.
For DVT prevention after surgery, doctors often prescribe short‑term anticoagulation plus mechanical methods:
- Compression stockings - graduated pressure promotes venous return.
- Intermittent pneumatic compression devices - inflatable cuffs that rhythmically squeeze the legs.
Patients with chronic clotting disorders may need lifelong anticoagulation, regular blood‑test monitoring, and lifestyle tweaks.

Practical Tips to Lower Your Own Risk
Even if you’re not a medical professional, you can adopt habits that keep blood flowing:
- Stand up and walk every 1-2 hours during long trips or desk work.
- Hydrate well; dehydration makes blood thicker.
- Maintain a healthy weight - excess fat puts extra pressure on veins.
- Talk to your doctor before starting hormone therapy if you have a family history of clotting.
- If you’ve had a previous DVT, keep your follow‑up appointments and never stop prescribed anticoagulants without guidance.
When to Seek Immediate Help
Sudden, sharp chest pain, rapid heartbeat, coughing up blood‑streaked sputum, or unexplained shortness of breath are red‑flag signs of a massive PE. Call emergency services right away-time is the difference between a quick recovery and a life‑threatening event.
| Risk Factor | Predominant for DVT | Predominant for PE |
|---|---|---|
| Immobility | ✓ | ✓ (indirect) |
| Recent Surgery | ✓ | ✓ (especially orthopedic) |
| Genetic Disorder (e.g., Factor V Leiden) | ✓ | ✓ (if clot travels) |
| Cancer | ✓ | ✓ (high‑grade tumors) |
| Hormone Therapy | ✓ | ✓ (if embolization) |
Frequently Asked Questions
Can a small DVT cause a serious PE?
Yes. Even a clot that seems minor in the calf can travel to the lungs. Size matters less than location; a fragment that blocks a major pulmonary artery can be life‑threatening.
How long do I need to stay on anticoagulants after a PE?
Typical treatment lasts 3‑6 months for a first‑time PE without underlying risk factors. If you have a persistent clotting disorder, lifelong therapy may be recommended.
Is it safe to fly after being treated for DVT?
Most doctors clear patients after at least 1‑2 weeks of stable anticoagulation and symptom resolution. Wearing compression stockings and moving every hour during the flight further reduces risk.
What does a "negative" D‑dimer result mean?
A negative result (below the assay’s cutoff) makes the presence of an active clot unlikely, allowing doctors to skip imaging in low‑risk patients.
Can lifestyle changes replace medication for DVT prevention?
Lifestyle measures-regular exercise, weight control, staying hydrated-significantly lower risk, but they don’t replace prescribed anticoagulants for high‑risk patients.



It is a well‑known fact that the medical establishment hides the true scale of venous thromboembolism behind a veil of bureaucratic jargon, a veil that only the enlightened few are permitted to see through.
When you examine the cascade of events leading from a stagnant clot in the calf to a catastrophic embolus in the pulmonary artery, you realize that the very notion of “random” clot formation is a myth perpetuated by pharmaceutical conglomerates to sell anticoagulants.
The immobility of modern life, enforced by governmental mandates for extended travel and sedentary work, creates the perfect breeding ground for silent clots that the mainstream media never dares to mention.
Moreover, the so‑called “D‑dimer” test is a crude proxy that masks deeper metabolic disruptions that only a specialist in hemostasis can decode, yet the average physician is content to rely on a single number.
These hidden pathways are deliberately obfuscated because the profit margins on direct oral anticoagulants dwarf any public health benefit of genuine prevention.
Consider the fact that compression stockings are marketed as a panacea while the underlying genetic predispositions, such as Factor V Leiden, remain untreated, a strategy that funnels patients into a lifelong dependency on costly medication.
The very imaging modalities, CT pulmonary angiography and compression ultrasonography, are advertised as “gold standards” while the radiation exposure and false‑positive rates are conveniently downplayed.
In truth, the embolization process is a deterministic outcome of venous stasis, endothelial injury, and hypercoagulability-three pillars that the layperson can understand without resorting to the mystifying language of modern medicine.
If you step back and view the entire cascade as a controlled experiment, you see that the “risk factors” listed in popular articles are merely a checklist to keep you compliant with the pharmaceutical agenda.
Traveling on long‑haul flights, undergoing surgery, or taking hormone therapy are all predictable triggers that the industry uses to market their products, not unexpected anomalies.
The narrative of “sudden” pulmonary embolism is thus a manufactured drama designed to create fear and sell prophylactic devices such as pneumatic compression boots, which generate revenue for the manufacturers.
Furthermore, the recommendation to “stay hydrated” is a simplistic platitude that ignores the complex interplay of plasma viscosity, platelet activation, and inflammatory cytokines that truly govern clot formation.
When you parse the literature with a critical eye, you discover that lifestyle modifications, while beneficial, are insufficient without the hidden hand of anticoagulation therapy gently nudged upon you by your physician.
Therefore, the prudent individual must cultivate a skeptical mindset, demand full disclosure of test sensitivities, and question the relentless push for medication, lest they become pawns in a profit‑driven health paradigm.
The only way to truly mitigate the risk is to adopt a holistic approach that integrates movement, genetic screening, and a critical appraisal of the medical narrative, thereby reclaiming agency over one’s circulatory health.