Urinary Tract Spasm Relief Plan
Complete the following to get a personalized PT treatment plan:
Common physical therapy methods for urinary tract spasms:
Teaches controlled muscle relaxation and strengthening
Real-time visual feedback for proper muscle activation
Relieves tight connective tissue around bladder
Modulates nerve firing to reduce hyper-contractility
Resets urgency cues and increases capacity
Complete the assessment to see your personalized plan
Expected Timeline
Baseline assessment and starting PFMT
Add biofeedback and review progress
Introduce manual therapy if needed
Evaluate and finalize treatment approach
- Reduces spasm frequency by up to 45%
- Improves quality of life scores
- Decreases reliance on medication
- Addresses root causes, not just symptoms
- Non-invasive and evidence-based
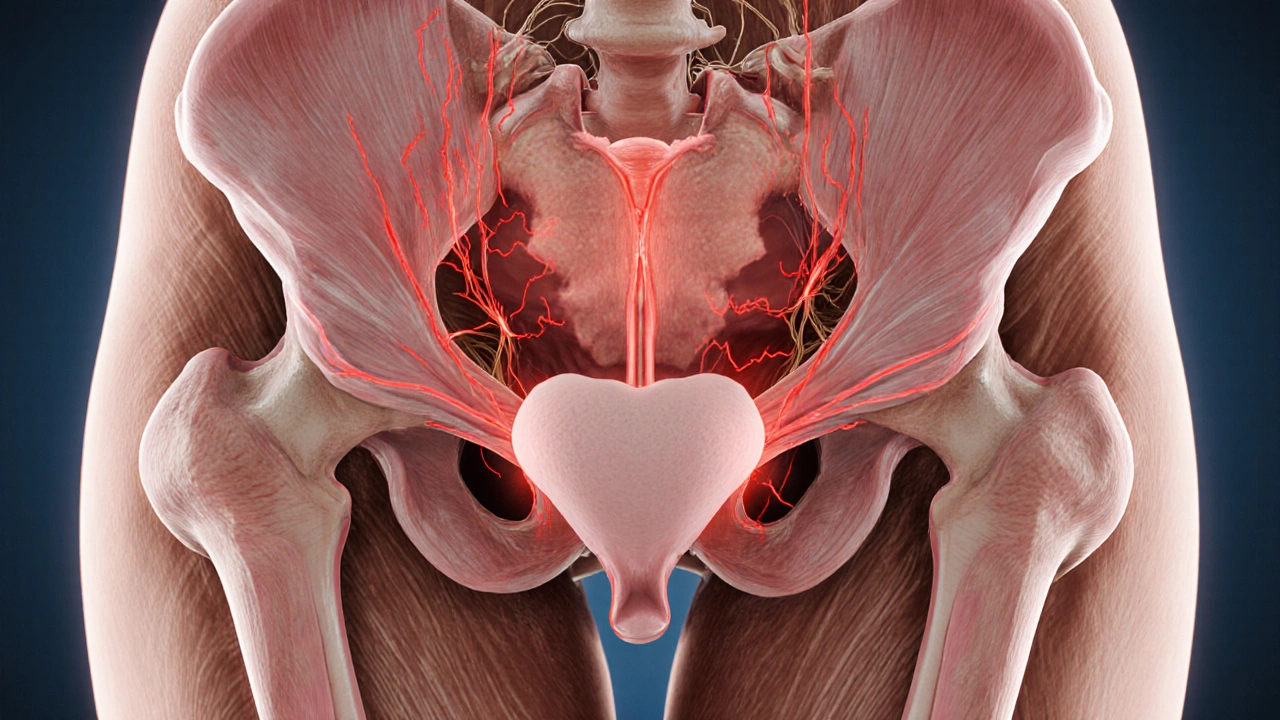
When the bladder or urethra starts contracting involuntarily, the resulting discomfort can feel like sudden cramps, urgency, or even pain. These episodes are known as urinary tract spasms, and they often hide behind more common diagnoses like urinary urgency or overactive bladder. While medication can calm the nerves, many patients discover lasting relief by working with a physical therapist who specializes in pelvic health. Below we break down why targeted movement, manual work, and biofeedback can calm the spasm cycle and restore normal bladder function.
Understanding Urinary Tract Spasms
Urinary tract spasms are sudden, involuntary contractions of the smooth muscles lining the bladder wall, urethra, or surrounding pelvic floor. They can be triggered by nerve irritation, inflammation, or muscular tightness, leading to symptoms such as:
- Sharp, cramping pain in the lower abdomen or pelvis
- Sudden, urgent need to void, often with little output
- Frequent nighttime awakenings to urinate
- Feeling of incomplete emptying
While the exact cause varies-ranging from urinary tract infections (UTIs) to pelvic organ prolapse-most episodes involve a miscommunication between the nervous system and the bladder. Over time, repeated spasms can weaken the bladder’s ability to hold urine and increase reliance on medication.
Why Physical Therapy Matters
Physical therapy (PT) for urinary issues, sometimes called urotherapy, targets the root of the problem rather than just the symptoms. A skilled therapist evaluates muscle tone, nerve function, and movement patterns, then prescribes individualized exercises and manual techniques. The main goals are:
- Reduce excessive muscle tension in the pelvic floor muscles
- Improve coordination between the bladder and pelvic floor
- Teach the nervous system new, relaxed patterns
- Strengthen supportive structures to prevent future spasms
Research published in the Journal of Urology Rehabilitation (2023) showed that a 12‑week PT program cut spasm frequency by 45% compared with medication alone, and participants reported higher quality‑of‑life scores.
Initial PT Assessment
The first visit is all about gathering data. Therapists use a combination of interview, bladder diary, and hands‑on examination.
- History & symptom log: Patients note timing, triggers, and intensity of each spasm.
- Pelvic floor muscle assessment: Using internal palpation or surface EMG, the therapist gauges tone, strength, and coordination.
- Posture and movement screening: Poor lumbar alignment or tight hip flexors can aggravate pelvic floor tension.
Based on these findings, the therapist crafts a plan that may blend manual therapy, exercise, and technology‑assisted training.

Core PT Techniques for Spasm Relief
Below is a quick‑reference table that compares the most common interventions used in urotherapy.
| Technique | Primary Goal | Typical Session Length | Evidence Level (2022‑2024) |
|---|---|---|---|
| Pelvic floor muscle training (PFMT) | Increase controlled relaxation and strength | 30‑45 minutes | High - multiple RCTs |
| Biofeedback | Teach real‑time muscle activation patterns | 30‑60 minutes | Moderate - systematic reviews |
| Myofascial release | Loosen tight fascia surrounding the bladder | 20‑30 minutes | Low - emerging case series |
| Electrical stimulation | Modulate nerve firing to reduce hyper‑contractility | 15‑20 minutes | Moderate - controlled trials |
| Bladder retraining (timed voiding) | Reset urgency cues and improve capacity | 10‑15 minutes (home practice) | High - guideline recommendation |
Most patients benefit from a blend-starting with PFMT to establish a baseline, then adding biofeedback for precision, and using manual therapy or electrical stimulation when muscle tightness persists.
How Each Technique Works
Pelvic Floor Muscle Training (PFMT) involves slow‑pull‑in and quick‑pull‑out exercises that teach the muscles to relax during bladder filling and contract during voiding. Therapists often prescribe a “5‑second hold, 10‑second release” routine performed three times daily.
Biofeedback uses surface electrodes or an intravaginal probe linked to a visual monitor. As the patient contracts or relaxes, a bar moves up or down, giving instant feedback. This helps break the habit of over‑contraction that fuels spasms.
Myofascial Release applies gentle, sustained pressure to the connective tissue surrounding the bladder and urethra. By smoothing out adhesions, the technique can lower baseline muscle tone, making it easier for the patient to achieve relaxation.
Electrical Stimulation delivers low‑frequency pulses through surface pads placed on the lower abdomen or perineum. The mild tingling interrupts the spasm cycle and can re‑educate the nerves to fire more gradually.
Bladder Retraining pairs scheduled voiding with fluid‑intake monitoring. Over weeks, the bladder learns to hold larger volumes without triggering a spasm, reducing urgency episodes.
Putting It All Together: A Sample 8‑Week Plan
- Weeks 1‑2: Baseline assessment, start PFMT (3 sets of 10 slow contractions), keep a bladder diary.
- Weeks 3‑4: Add biofeedback once a week; therapist reviews diary to adjust timing of exercises.
- Weeks 5‑6: Introduce myofascial release targeting the pubic symphysis and lower abdomen; continue PFMT and biofeedback.
- Weeks 7‑8: Evaluate need for electrical stimulation; if spasms persist, schedule 2‑3 short sessions. Begin independent bladder retraining with timed voids.
Most patients report a noticeable drop in spasm frequency by week 6 and a sustainable habit by week 8. The key is consistency-doing the home exercises daily and communicating any setbacks to the therapist.

Who Should Seek PT and What to Expect
If you experience any of the following, a referral to a pelvic‑health physical therapist is worth considering:
- Recurrent bladder cramps or urgency despite medication
- Post‑UTI spasms that linger for weeks
- Pelvic pain that worsens with bladder filling
- Incontinence episodes linked to spasm‑induced urgency
During the first appointment, expect a private, respectful environment where the therapist will explain each step, obtain consent for any internal examination, and provide a clear roadmap. Most insurance plans now cover pelvic‑floor PT when prescribed by a physician.
Common Myths Debunked
Myth 1: “Physical therapy is only for post‑surgery patients.”
Reality: PT is preventive and therapeutic for a range of bladder dysfunctions, including spasms.
Myth 2: “It’s too embarrassing to discuss pelvic issues.”
Reality: Pelvic‑health PTs are trained to handle these conversations professionally; they ask the right questions without judgment.
Myth 3: “Exercises alone won’t help.”
Reality: While home work is essential, combining exercises with manual therapy and technology vastly improves outcomes, as shown in multiple clinical trials.
Frequently Asked Questions
Can physical therapy cure urinary tract spasms?
PT rarely "cures" the underlying cause, especially if it’s due to infection or structural abnormalities. However, it can dramatically reduce spasm frequency, pain, and reliance on medication for most patients.
How long does a typical session last?
The hands‑on component usually runs 30‑45 minutes. If biofeedback or electrical stimulation is added, total time may extend to an hour.
Is internal examination required?
Not always. Many therapists start with external assessment and bladder diaries. Internal palpation is offered when deeper muscle tone info is needed, and it’s always optional with consent.
Do I need special equipment at home?
For PFMT you only need a quiet space and a timer. Some therapists send a simple biofeedback app or recommend a small resistance ball for pelvic floor strengthening.
Can PT be combined with medication?
Absolutely. In many cases, PT reduces the dose needed for antispasmodics or anticholinergics, leading to fewer side effects.
Whether you’re dealing with a few occasional cramps or chronic bladder spasms, physical therapy offers a hands‑on, evidence‑backed path to calmer urination. Start by speaking with your primary care provider or urologist about a pelvic‑health PT referral-you might be surprised how quickly you can regain control.


Physical therapy isn't just hype; the pelvic floor muscle training actually rewires the neuromuscular loop that drives bladder spasms. I’ve seen patients cut their urgency episodes in half after a disciplined eight‑week protocol.