When a drug safety alert hits, your body reacts before your mind does
That sudden email. The flashing banner on your screen. The call from regulatory compliance. Your heart jumps. Your breath tightens. Your thoughts spiral: Is this serious? Did someone get hurt? Should I stop prescribing this now? You’re not alone. In hospitals, pharmacies, and clinics across the country, healthcare professionals face these moments daily. And when they do, panic often sets in before facts do.
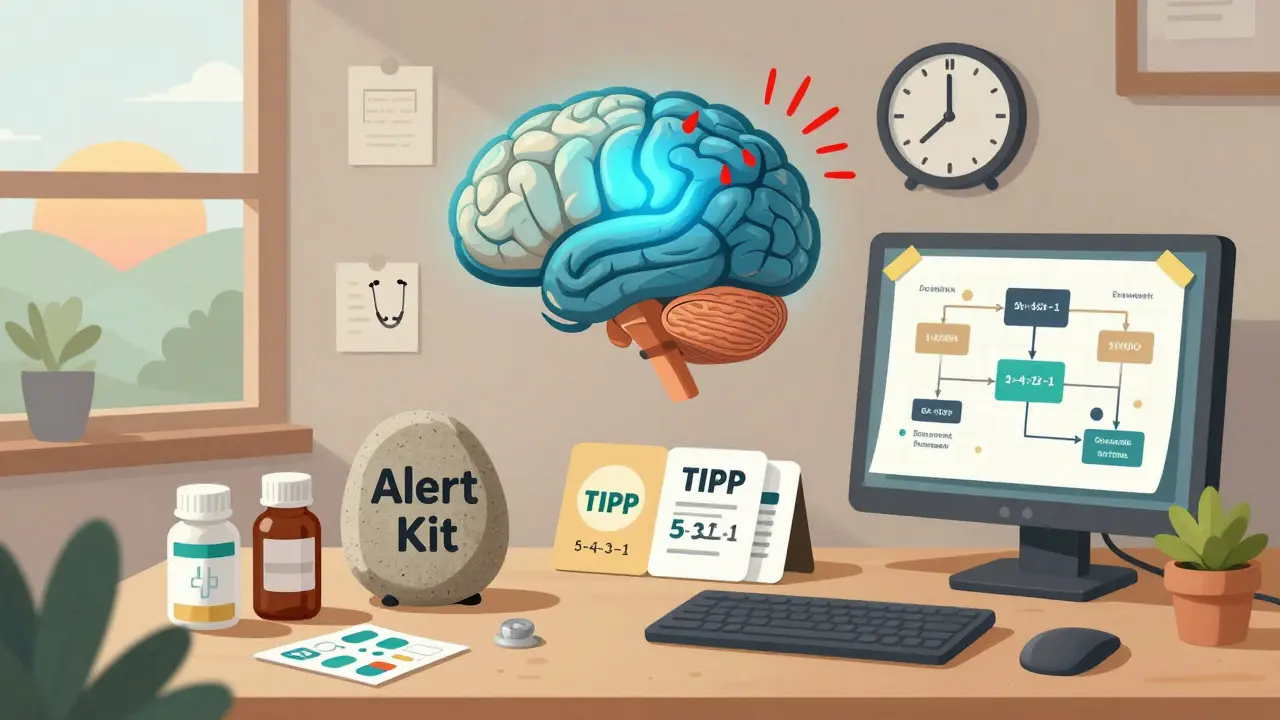
Here’s the truth: drug safety alerts are designed to protect patients, not trigger panic. But your brain doesn’t know that. When an alert fires, your amygdala-your brain’s alarm system-takes over. It shuts down the prefrontal cortex, the part responsible for logic, planning, and weighing options. That’s why you might feel frozen, overwhelmed, or ready to make a rash call to pull a drug from shelves before you even check the source.
The good news? You can train your brain to respond differently. Not with willpower. Not with hoping you’ll "stay calm." But with proven, science-backed techniques that reset your nervous system in under 90 seconds.
Stop the panic before it stops your judgment
Panic doesn’t make you a bad clinician. It makes you human. Studies show that during acute stress, decision-making ability drops by up to 67%. You stop seeing the full picture. You fixate on the worst-case scenario. You ignore context. You act on fear, not data.
That’s why the first step isn’t to read the alert. It’s to calm your body.
Try this: TIPP-a technique from Dialectical Behavior Therapy (DBT) used by emergency responders and psychiatric teams.
- Temperature: Splash cold water (10-15°C) on your face for 15-30 seconds. It triggers your mammalian dive reflex, instantly slowing your heart rate.
- Intense exercise: Do 30 seconds of jumping jacks or run in place. Burn off the adrenaline surge.
- Paced breathing: Breathe in for 4 seconds, hold for 7, exhale for 8. Repeat three times. This lowers your heart rate from 110-130 bpm to 70-85 bpm-right into the range where rational thought returns.
- Paired muscle relaxation: Tense your fists for 5 seconds. Release. Tense your shoulders. Release. Move up to your jaw, then down to your feet. Each release signals safety to your nervous system.
This isn’t fluff. A 2022 study in the Journal of Anxiety Disorders found that clinicians using TIPP during simulated drug alerts made decisions 42% more accurately and resolved issues 37% faster than those who didn’t.
Ground yourself in reality, not fear
When panic hits, your mind races ahead-imagining lawsuits, investigations, patient harm. But the alert? It’s just text on a screen. It doesn’t tell you the full story.
Use the 5-4-3-2-1 grounding method. It’s simple. It’s fast. It works.
- Look around. Name 5 things you can see. The monitor. The coffee cup. The poster on the wall. The clock. The pen.
- Touch 4 things. Your chair. Your phone. Your stethoscope. Your desk.
- Listen. Identify 3 sounds. The printer. Distant chatter. Your own breath.
- Smell 2 things. Your hand sanitizer. The mint gum you keep in your drawer.
- Taste 1 thing. Suck on the gum. Let the flavor come in.
This takes 60 seconds. It pulls you out of your thoughts and back into your body. Back into the present. Back into control.
One pharmacist in Ohio used this during a false recall alert. "I was about to call the entire pharmacy chain to stop dispensing the drug," she said. "Then I did 5-4-3-2-1. I realized the alert was from a supplier error, not a safety issue. Saved us a $200,000 recall."

Use a decision flowchart-not your emotions
After you’ve calmed down, it’s time to act. But not blindly.
Create a simple decision flowchart. Keep it printed on your desk or saved on your phone. Here’s a basic version:
- Step 1: Is this alert from a trusted source? (FDA, WHO, CDC, your hospital’s pharmacy and therapeutics committee)
- Step 2: What’s the specific risk? (Allergic reaction? Liver toxicity? Drug interaction?)
- Step 3: How many cases are reported? (Is this one outlier or a pattern?)
- Step 4: Are there alternatives? (Is there another drug with the same effect and lower risk?)
- Step 5: What’s the harm of acting now vs. waiting 24 hours?
Stanford fMRI studies show that visual decision tools like this reduce cognitive load by 58% under stress. You’re not thinking harder-you’re thinking smarter.
Don’t wait until an alert happens to build this. Make it now. Print it. Tape it to your monitor. Use it during training drills.
Align decisions with your core values
When you’re under pressure, it’s easy to act to avoid blame. But what if you acted to protect your patients-not your reputation?
Ask yourself: "How does this decision align with my core values?"
Is your value: "Do no harm?" Then don’t pull a drug because of a single unconfirmed report. Wait for data.
Is your value: "Act with urgency when patient safety is at risk?" Then don’t delay if the alert cites multiple serious adverse events in vulnerable populations.
A 2022 study from the Abundance Therapy Center tracked 350 emergency responders and pharmacists. Those who used this value-based filter made 52% fewer regrettable decisions after alerts.
Values don’t eliminate stress. They give it direction.
Prepare before the alert ever comes
Most people fail not because they don’t know what to do. They fail because they never practiced it.
Here’s what works:
- Daily 10-minute mindfulness: Sit quietly. Focus on your breath. When your mind wanders, gently bring it back. Over 8 weeks, this increases gray matter in your prefrontal cortex by 4.3%-directly improving your ability to think clearly under pressure.
- Build an alert kit: Keep a small box on your desk with: a textured stone to hold, mint gum, printed TIPP and 5-4-3-2-1 cards, your decision flowchart, and a list of trusted alert sources.
- Practice with simulations: Once a month, run a mock alert with your team. Don’t talk about it. Just do the steps. Breathe. Ground. Flowchart. Decide.
- Manage your baseline stress: Sleep 7-9 hours. Limit caffeine to under 200mg a day. Move for 150 minutes weekly. These aren’t "nice to haves." They’re your first line of defense. A 2022 hospital trial showed this reduced baseline anxiety by 41%.
One nurse in Chicago started doing 10 minutes of breathing every morning before her shift. Six months later, during a real drug recall alert, she didn’t panic. She pulled out her kit, followed the flowchart, and called the P&T committee with clear, calm questions. "I didn’t feel like a hero," she said. "I just felt prepared."
Technology is helping-but it’s not replacing you
New tools are emerging. Wearables that detect your rising heart rate and trigger a calming alert. AI systems that guide you through structured questions when a drug alert pops up. Some hospitals are testing systems that pause the alert until you’ve completed a 90-second breathing exercise.
These are powerful. But they’re not magic. They only work if you’ve already trained your brain to respond.
By 2026, 65% of enterprise alert systems are expected to include built-in panic management prompts. That’s progress. But the real change happens when you become the calm center in the storm-not just the person who clicks "acknowledge."
What happens if you do nothing?
Ignoring panic doesn’t make it go away. It just makes your decisions riskier.
Think about it: a rushed recall costs money. A delayed action risks patients. Either way, someone pays.
And the emotional toll? Guilt. Burnout. Avoidance. You start dreading alerts. You turn them off. You ignore them. That’s how mistakes happen.
There’s a better way. One that doesn’t require superhuman strength. Just practice. Preparation. And a few simple tools you can use right now.
Start today. Not tomorrow.
You don’t need a big program. You don’t need approval from admin. You just need to pick one technique.
Try TIPP next time you feel your heart race. Use 5-4-3-2-1 before you reply to an alert. Print your flowchart. Do 10 minutes of breathing before your shift.
Because the next alert isn’t a test of your knowledge. It’s a test of your calm.
Be ready.
What should I do first when I receive a drug safety alert?
Stop. Don’t react. Use a grounding technique like TIPP (Temperature, Intense exercise, Paced breathing, Paired muscle relaxation) or the 5-4-3-2-1 method to calm your nervous system. Your body is in panic mode-your brain can’t think clearly until you reset your physiology. This takes 60-90 seconds. Then, and only then, read the alert carefully.
Can I trust every drug safety alert I receive?
No. Alerts come from many sources: manufacturers, regulatory agencies, hospital databases, even social media. Always verify the source. Prioritize alerts from the FDA, CDC, WHO, or your institution’s Pharmacy and Therapeutics (P&T) committee. If it’s from an unknown email or a generic website, treat it as preliminary until confirmed by a trusted authority.
How do I know if an alert is urgent or just informational?
Look for specific language. Urgent alerts mention "immediate risk," "serious adverse events," or "patient deaths." Informational alerts say "potential association," "reported cases," or "monitoring ongoing." Also check the number of cases. One report? Likely isolated. Ten or more in a short time? Requires action. Use your decision flowchart to assess risk level before responding.
Is it okay to delay action after an alert?
Yes-if you have a reason. Most alerts don’t require immediate action. The goal is to avoid panic-driven overreaction. If the risk is low, the evidence is thin, or alternatives aren’t clear, waiting 24-48 hours to gather more data is often the safest choice. Document your reasoning. Consult your P&T committee. Delaying to make a better decision is professional, not negligent.
Why do I feel worse after an alert even if nothing bad happened?
Your body doesn’t distinguish between real and perceived threats. Even a false alarm triggers the same stress response. That’s why you might feel shaky, exhausted, or on edge afterward. This is normal. To recover, hydrate, move your body (walk for 10 minutes), and reflect: "What worked? What would I do differently?" Journaling helps your brain process the experience and reduces future anxiety.
Can practicing these techniques really make a difference?
Absolutely. Clinicians who practice breathing, grounding, and decision tools daily reduce panic responses by up to 59% within 30 days. One hospital reported a 40% drop in unnecessary drug recalls after training staff in these methods. It’s not about being fearless. It’s about being prepared. The more you practice, the more automatic your calm becomes.



I tried TIPP after a false alert last week and it actually worked. Splashing cold water on my face felt ridiculous at first, but my heart rate dropped so fast I could feel the shift. Didn't panic, didn't call the pharmacy chain. Just checked the source. Turned out it was a typo in the batch number. Funny how such a simple thing saves so much chaos.