Drug Interaction Checker
Check if your medications might interact dangerously before starting a new one. This tool demonstrates common interactions based on medical guidelines.
Select two medications to check for interactions.
This tool demonstrates common interactions based on medical guidelines. It is not a substitute for professional medical advice. Always consult your pharmacist or doctor for personalized guidance.
Every year, thousands of people end up in the hospital because they took two medications that shouldn’t have been mixed. Some of these cases are preventable. The problem isn’t always bad doctors or careless pharmacists-it’s often a simple gap in communication. You start a new pill, maybe for high blood pressure or depression, and don’t realize it could react dangerously with the statin you’ve been taking for years, or that grapefruit juice could turn your medicine into a toxin. This isn’t rare. Studies show up to half of all adverse drug reactions can be avoided if people check for interactions before starting a new medication.
Why Drug Interactions Are More Dangerous Than You Think
Drug interactions don’t just mean one pill makes another less effective. They can turn harmless drugs into life-threatening combinations. For example, mixing simvastatin (a cholesterol drug) with amiodarone (a heart rhythm medication) can increase the risk of muscle breakdown by 15 times. That’s not a minor side effect-it can lead to kidney failure or death. Even foods can cause trouble. Grapefruit juice blocks enzymes in your liver that break down over 85 medications, including some statins, blood pressure pills, and anti-anxiety drugs. One glass can make your drug dose dangerously high. The FDA estimates that preventable drug reactions cause about 7,000 deaths in the U.S. each year. Many of these happen because patients don’t tell all their doctors about every medication they take. People on multiple prescriptions often see four or more different providers. Each one writes a new script without knowing what the others prescribed. That’s why checking for interactions isn’t just a good idea-it’s a survival step.Step 1: Make a Complete Medication List
Start by writing down everything you take. Not just prescriptions. Include over-the-counter painkillers like ibuprofen or naproxen, sleep aids, antacids, vitamins, herbal supplements, and even CBD oil. Write the exact name, dosage, and how often you take it. Don’t guess. If you’re not sure, open your pill bottles and check the labels. A 2018 study found that bringing all your physical meds to a doctor’s appointment cuts medication errors by 37%. Example: If you take lisinopril 10 mg once daily, metformin 500 mg twice a day, melatonin 3 mg at bedtime, and fish oil 1,000 mg daily-list them all. Don’t assume your doctor knows you take melatonin because you bought it at the grocery store. They might not ask. You have to tell them.Step 2: Ask the Right Questions Before Taking Anything New
When your doctor or pharmacist suggests a new drug, don’t just say “okay.” Ask these four questions out loud:- Can I take this with my other medications?
- Should I avoid any foods, drinks, or alcohol with this?
- What are the warning signs of a bad reaction I should watch for?
- How does this drug affect my body differently because of what else I’m taking?
Step 3: Use a Trusted Drug Interaction Checker
There are free, reliable tools online that can help you spot problems before you even leave the pharmacy. The Drugs.com Drug Interactions Checker is one of the most accurate. It checks over 24,000 prescription drugs, 7,000 supplements, and 4,000 foods. In a 2021 study, it caught 92.4% of clinically significant interactions-better than WebMD and close to the University of Liverpool’s HIV-specific tool, which is considered the gold standard. But here’s the catch: no tool is perfect. The FDA warns these apps don’t know your kidney function, age, weight, or genetics. Two people taking the same drugs might react completely differently. Use these tools as a warning system-not a final answer. Always double-check with your pharmacist.
Step 4: Know the High-Risk Combinations
Some drug pairs are so dangerous they show up in medical guidelines as red flags. The American Academy of Family Physicians identified seven combinations responsible for 63% of serious interaction hospitalizations:- Warfarin + NSAIDs (like ibuprofen or naproxen)
- SSRIs (like sertraline) + MAOIs (like phenelzine)
- Digoxin + clarithromycin (an antibiotic)
- Statins (like simvastatin) + fibrates (like fenofibrate)
- Calcium channel blockers + protease inhibitors (used for HIV)
- Sildenafil (Viagra) + nitrates (like nitroglycerin)
- Theophylline + fluvoxamine (an antidepressant)
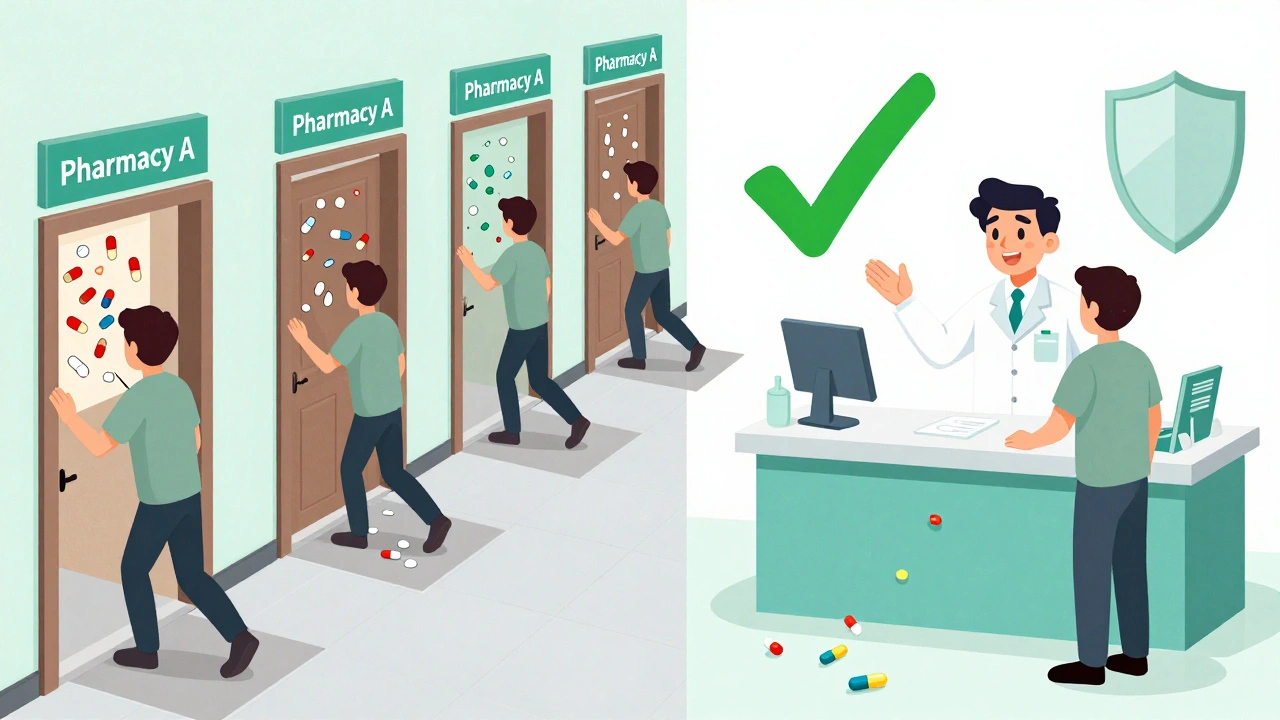
Step 5: Stick to One Pharmacy
Using multiple pharmacies is one of the biggest risks. If you get your blood pressure med from one store, your painkiller from another, and your supplements from a third, no one has the full picture. A 2021 study of 22,000 Medicare patients found that using just one pharmacy cuts serious drug interactions by 31%. Pharmacists are trained to catch interactions. But they can’t do it if they don’t see all your prescriptions. If you’re switching pharmacies because of cost, ask your current pharmacy to transfer your records. Most will do it for free. The BeMedWise Program calls this the “One Pharmacy Rule.” It’s simple, cheap, and life-saving.Step 6: Keep a Medication Passport
Create a one-page document-digital or printed-that lists every medication you take. Update it after every doctor’s visit, ER trip, or pharmacy refill. Include:- Drug name and dose
- Why you take it
- When you take it
- Any side effects you’ve noticed
Step 7: Watch for Warning Signs
Once you start a new drug, pay attention to your body. The first 48 hours are critical. Many dangerous interactions show up quickly. Look out for:- Unusual muscle pain or weakness (could mean rhabdomyolysis)
- Unexplained bruising or bleeding (could mean blood thinning)
- Rapid heartbeat, dizziness, or fainting
- Severe nausea, vomiting, or diarrhea
- Sudden confusion or mood changes
Why Technology Isn’t Enough
Hospitals and pharmacies use computer systems to flag interactions. But in 2022, pharmacists still filled 8.3% of prescriptions with known dangerous combinations. Why? Because too many alerts lead to “alert fatigue.” If your system pops up 12 warnings for every prescription, you start ignoring them. One Reddit user said they stopped reading alerts after getting 12 false positives in a row-then missed a real warning. Also, many systems don’t account for your genetics. Some people metabolize drugs slowly because of their CYP450 enzyme profile. The NIH is testing ways to include this data in interaction checkers-and early results show accuracy improves by 37%. But that tech isn’t mainstream yet. So you still have to be your own advocate.What You Can Do Today
You don’t need to wait for your next appointment. Right now:- Grab all your pill bottles and make a list.
- Go to Drugs.com and enter every item on your list.
- Call your pharmacy and ask if they’ve flagged any interactions.
- Next time you see a doctor, hand them your list and ask: “Could any of these react badly with what you’re prescribing?”
Can I trust online drug interaction checkers?
Yes, but not completely. Tools like Drugs.com and the University of Liverpool’s checker are highly accurate and updated daily. They catch most serious interactions. But they don’t know your kidney function, age, weight, or genetic makeup. Always use them as a first check, then confirm with your pharmacist or doctor. Never rely on them alone.
Do herbal supplements cause drug interactions?
Absolutely. Many people think supplements are harmless because they’re “natural,” but that’s not true. St. John’s Wort can make birth control, antidepressants, and blood thinners ineffective. Garlic, ginkgo, and ginseng can increase bleeding risk when taken with warfarin. Even vitamin K can reduce the effect of blood thinners. Always list every supplement you take-no matter how small.
What should I do if my doctor says a combination is safe but the app says it’s dangerous?
Ask for clarification. Say: “I saw a warning on Drugs.com about this combination. Can you explain why you think it’s safe for me?” Sometimes, the doctor knows your history and has a good reason. Other times, they missed it. Either way, you deserve a clear answer. If they dismiss your concern without explanation, get a second opinion.
Can grapefruit really make my medication dangerous?
Yes. Grapefruit juice blocks an enzyme in your liver called CYP3A4, which breaks down many drugs. This causes the drug to build up in your blood to dangerous levels. It affects statins (like simvastatin), some blood pressure meds, anti-anxiety drugs, and even some cancer treatments. One glass can have an effect for up to 72 hours. If you’re on any of these drugs, avoid grapefruit entirely-even small amounts.
Why do I keep getting alerts for interactions that aren’t real?
That’s called “alert fatigue.” Many electronic systems flag every possible interaction, even theoretical ones. A 2022 study found that 65% of alerts in hospitals are low-risk or false. Pharmacists and doctors get so many that they start ignoring them. Don’t assume a warning is wrong just because it’s common. If you see a “major” or “contraindicated” alert, investigate it-even if it’s happened before.
Is it safe to take new meds if I’ve taken them before without problems?
Not necessarily. Your body changes. Your liver or kidney function might be different now. You might be taking a new supplement or eating more grapefruit. You might have gained weight or started a new condition like high blood pressure. What was safe last year might not be safe today. Always check before restarting or adding anything-even if you’ve used it before.



Man, this is straight-up life-saving info. I never thought about my turmeric supplements messing with my blood thinner. Gonna make a list tonight and check everything on Drugs.com. Thanks for laying it out so simple.