Every year, tens of thousands of pets end up in emergency vet clinics because they ate something they shouldn’t have-and the biggest culprit isn’t chocolate, grapes, or even trash. It’s your medicine. A dog snatches a pill off the nightstand. A cat licks residue off a counter where you dropped a capsule. In seconds, a routine morning turns into a life-or-death situation. Human medications are the #1 cause of pet poisonings in the U.S., with over 150,000 cases reported annually. And the worst part? Most of these incidents are preventable-if you know what to look for.
Why Human Medications Are So Dangerous for Pets
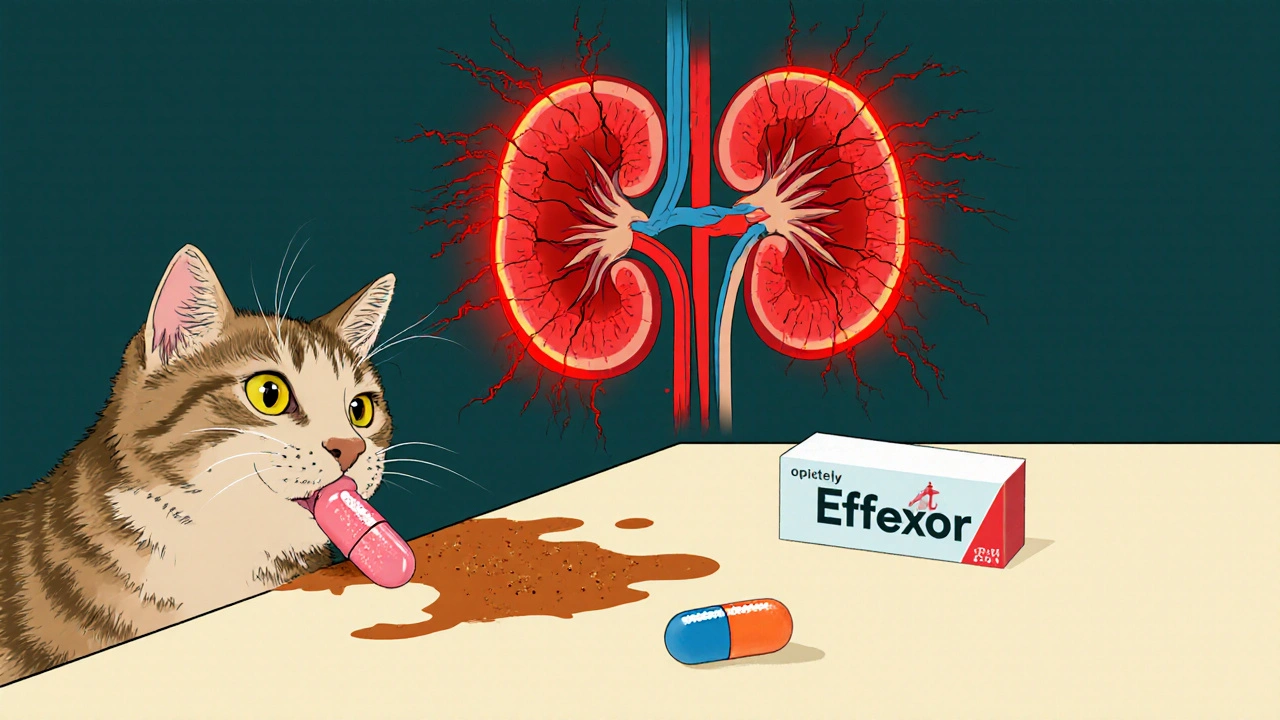
What’s safe for you can be deadly for your pet. Dogs and cats don’t process drugs the same way humans do. Their livers and kidneys weren’t built to handle the concentrations found in human pills. A single 20mg dose of ibuprofen can cause stomach ulcers in a 20-pound dog. One 37.5mg Effexor capsule can send a cat into liver failure. Even a small amount of Adderall can spike a dog’s heart rate past 220 beats per minute-normal is 60-140.
It’s not just about the dose. It’s about the type of drug. Antidepressants, ADHD meds, painkillers, and sleep aids are the most common offenders. And pets don’t care if it’s a slow-release tablet or a chewable. If it tastes sweet or smells familiar, they’ll eat it. In fact, 63% of feline cases involve cats consuming entire bottles because of the sugary coating on pills like Effexor.
Top 4 Medication Types That Cause Overdose in Pets
1. Antidepressants (SSRIs and SNRIs)
Drugs like Prozac, Lexapro, and Effexor are common in households-and deadly in pets. These medications cause serotonin syndrome, a dangerous overstimulation of the nervous system.
- Signs: High fever (103-106°F), pacing, whining, tremors, seizures
- Timeline: Symptoms appear within 30 minutes to 12 hours
- Key red flag: A dog that’s normally calm suddenly acts frantic, vocal, and disoriented
Effexor is especially dangerous for cats. Just one capsule can cause liver enzyme levels to spike above 1,200 U/L (normal is 10-100). In dogs, SSRIs like Prozac have a slightly wider safety margin, but toxic doses still start at 10-20mg/kg-far below what’s prescribed to humans.
2. ADHD Medications (Adderall, Concerta, Ritalin)
These are stimulants-amphetamines and methylphenidate. They’re designed to make humans more alert. In pets, they turn the nervous system into overdrive.
- Signs: Extreme hyperactivity, rapid breathing, tremors, heart rate over 220 bpm, body temperature above 107°F
- Timeline: Symptoms hit within 15-60 minutes
- Key red flag: Fixed, dilated pupils and a dog that’s shaking uncontrollably
A 20-pound dog eating one 20mg Adderall tablet is in critical condition. The average dog’s normal heart rate is 60-140 bpm. At 220+, the heart is at risk of arrhythmia or cardiac arrest. These cases require immediate treatment-delaying by even an hour can be fatal.
3. Painkillers (NSAIDs like Ibuprofen, Naproxen)
These are the most common cause of pet poisonings overall. People think, “It’s just Advil,” but dogs and cats can’t break down these drugs safely.
- Signs: Vomiting (92% of cases), black tarry stools (melena), loss of appetite, lethargy, increased thirst or urination
- Timeline: GI symptoms start in 1-6 hours; kidney failure can develop in 24-72 hours
- Key red flag: The classic triad-vomiting, bloody stools, and sudden lethargy
Dogs can tolerate small doses of ibuprofen (5-10mg/kg), but anything over 50mg/kg is toxic. Cats? They’re far more sensitive. Just 5mg/kg can cause kidney damage. BUN levels above 120 mg/dL (normal: 10-25) mean acute kidney failure is already underway.
4. Acetaminophen (Tylenol)
This is the most species-specific poison. It’s less dangerous for dogs-but lethal for cats.
- Signs in cats: Brown or blue gums (methemoglobinemia), swelling in face/paws, difficulty breathing, vomiting, lethargy
- Signs in dogs: Lethargy, vomiting, jaundice (yellow gums), dark urine
- Timeline: Cats show symptoms in 1-4 hours; dogs in 24-72 hours
- Key red flag: Brown-tinged mucous membranes in cats = emergency
Cats lack the enzyme needed to detoxify acetaminophen. A single 10mg/kg dose can kill them. Dogs can handle up to 150mg/kg before liver damage occurs-but that’s still far less than a human dose. One 500mg tablet can be fatal to a small dog.
How to Recognize an Overdose Fast
Time is everything. Studies show 93% of pets survive if treatment starts within 2 hours. That’s why you need a quick, reliable checklist.
- Check for evidence. Look for spilled pills, chewed packaging, or residue on their mouth or paws. In 63% of cases, owners find physical proof.
- Take their temperature. Use a rectal thermometer. Normal is 100-102.5°F. Anything above 103.5°F suggests stimulant or SSRI toxicity.
- Look at their gums. Bright pink = normal. Blue or brown = acetaminophen poisoning. Pale = shock or internal bleeding.
- Check their pupils. Dilated pupils in a dog that’s not scared or excited? Likely ADHD meds.
- Time the symptoms. Did they start within 30 minutes? That’s stimulants. Within 2 hours? Antidepressants. After 6 hours? NSAIDs or acetaminophen.
Don’t wait for “all” the symptoms. One or two, combined with a known exposure, is enough to act.
Common Mistakes Owners Make
Most pet owners don’t realize how quickly things can go wrong. Here’s what often happens:
- Mistaking agitation for excitement. A dog pacing and whining? “They’re just happy!” Nope-it’s serotonin syndrome.
- Thinking tremors mean they’re cold. Shivering? Maybe. But if it’s rhythmic, uncontrollable, and paired with a high fever? It’s drug toxicity.
- Waiting to see if they “get better.” Pets don’t recover on their own from drug overdoses. Delaying care increases mortality from 4% to 28%.
- Assuming cats are safe because they’re “finicky.” Cats are the most vulnerable. They lick everything. They’re more sensitive. And they show symptoms later-when it’s too late.
A 2023 PetMD survey of 1,247 owners found 68% initially misinterpreted early signs. Over 40% thought serotonin syndrome agitation was “excitement.” Nearly 37% thought tremors were just “shivering.”
What to Do If You Suspect an Overdose
Don’t wait. Don’t Google. Don’t try to induce vomiting unless a vet tells you to.
- Call immediately. Contact your vet or the Pet Poison Helpline (1-800-213-6680). They handle over 400,000 cases a year and respond in under a minute.
- Have details ready. What medication? How much? When? What’s your pet’s weight? What symptoms are you seeing?
- Don’t give anything. No milk, no activated charcoal (unless directed), no home remedies. Some treatments can make things worse.
- Go to the vet. Even if your pet seems okay. Some toxins don’t show symptoms for hours. Bloodwork, IV fluids, and antidotes (like N-acetylcysteine for acetaminophen) are lifesaving.
One success story: A Labrador ate ibuprofen. The owner noticed vomiting, bloody stools, and lethargy within 90 minutes. They called the vet, got activated charcoal administered, and the dog made a full recovery. Another case: A cat ate Effexor. The owner waited 4 hours because they thought it was “just acting weird.” The cat spent 7 days in the hospital and nearly died.
How to Prevent Overdose
Prevention is easier than you think:
- Store all meds in high cabinets or locked containers-not on nightstands or bathroom counters.
- Never leave pills on tables, purses, or car consoles. Pets are fast and clever.
- Use child-proof caps. They’re not just for kids.
- Dispose of unused pills properly. Don’t flush them-take them to a pharmacy drop-off.
- Keep a list of all medications in your home, including doses and frequencies. It helps vets act faster.
- Teach kids not to give pets “medicine” or snacks from the medicine cabinet.
There’s also a new app from the American College of Veterinary Emergency and Critical Care that uses AI to help owners identify symptoms. It’s still new, but early results show 89% accuracy in recognizing overdose patterns.
Final Thoughts
You don’t need to be a vet to save your pet’s life. You just need to know what to look for-and act fast. Human medications are everywhere. Your pet doesn’t understand the difference between your painkiller and their treat. But you can. Recognizing the signs early isn’t just helpful-it’s the difference between a full recovery and a funeral.
If you’ve ever wondered why your vet always asks, “Did your pet get into any meds?” now you know. It’s not routine. It’s critical. And if you’re ever in doubt-call. Always call. Better safe than sorry.
Can a small amount of human medication kill a pet?
Yes. Even a single pill can be fatal. For example, one 37.5mg Effexor capsule can cause liver failure in a cat. A 20mg ibuprofen tablet can cause stomach ulcers and kidney damage in a small dog. Pets are far more sensitive than humans, and many medications have no safe dose for them.
What should I do if my pet ate medication but seems fine?
Call a vet or poison control center immediately. Many toxins don’t show symptoms for hours-or even days. Acetaminophen, for example, can take up to 72 hours to cause liver damage in dogs. Waiting for signs to appear increases the risk of permanent organ damage or death. Early intervention is always better.
Are cats more at risk than dogs?
Yes, in several key ways. Cats lack certain liver enzymes that help break down drugs like acetaminophen and NSAIDs, making them far more vulnerable. A dose that’s dangerous for a dog can be lethal for a cat. Also, cats are more likely to lick residue from surfaces or their paws, leading to accidental ingestion. Effexor and Tylenol are especially deadly to cats-even tiny amounts.
What are the most dangerous human medications for pets?
The top four are: 1) NSAIDs like ibuprofen and naproxen (most common cause of poisoning), 2) Antidepressants like Effexor and Prozac, 3) ADHD medications like Adderall and Ritalin, and 4) Acetaminophen (Tylenol), especially for cats. These four categories account for over 68% of all medication-related pet poisonings.
Can I give my pet human medicine if they’re sick?
Never. Human medications are not formulated for pets and can cause severe toxicity, organ failure, or death. Even aspirin or Benadryl-which some people think are safe-can be dangerous without proper dosing and veterinary guidance. Always consult your vet before giving any medication to your pet.



So let me get this straight-my dog eating my Adderall is more dangerous than me forgetting to pay my rent? Wow. I guess my cat’s obsession with licking my toothpaste is just a cute quirk compared to this. Also, why does everyone act like we’re all just negligent monsters? I keep my meds in a drawer. Not a vault. Not a Fort Knox. A drawer. And yet I’m supposed to be terrified every time I take a pill? 😒