When a patient is stable on a brand-name NTI drug like warfarin, levothyroxine, or phenytoin, switching to a generic version isn’t just a cost-saving move-it’s a clinical decision. These are not ordinary medications. A tiny change in blood levels-just 5% or 10%-can mean the difference between control and crisis. That’s why patient communication when switching NTI generics isn’t optional. It’s essential.
Why NTI Drugs Are Different
Narrow Therapeutic Index (NTI) drugs have a razor-thin margin between the dose that works and the dose that harms. For example, warfarin’s target INR range is 2 to 3. Go below 2, and clots can form. Go above 3, and bleeding risks spike. Phenytoin’s therapeutic range? 10 to 20 mcg/mL. One extra milligram per day, and you could trigger seizures or toxicity. Even small differences in how a generic version is absorbed can push a patient out of that safe window. The FDA doesn’t treat NTI generics like regular ones. While most generics must prove they deliver 80-125% of the brand’s blood levels, NTI drugs must meet a much tighter standard: 90-111.11%. For some, like levothyroxine, the bar is even higher-95-105% for AUC. These aren’t arbitrary numbers. They’re based on real-world data from thousands of patient studies. But patients don’t know that. And if you don’t explain it, they’ll assume all generics are the same.What Patients Are Really Worried About
When you say, “We’re switching you to a generic,” patients hear: “This might not work as well.” And honestly? That fear isn’t irrational. A 2017 survey found that 8-12% of patients with well-controlled epilepsy had seizures after switching from brand to generic antiepileptics. That’s not common-but it’s real. And when it happens, trust shatters. Patients also worry about consistency. “If I’ve been on the same pill for years, why change now?” They remember stories-friends who had bad reactions, online posts about generic failures. They don’t care that the FDA approved it. They care that their body felt different. Your job isn’t to argue. It’s to acknowledge.How to Start the Conversation
Don’t lead with the science. Start with empathy. Say this: “I know you’ve been doing well on your current medication. Switching isn’t something we do lightly. But the generic version we’re moving to has been tested to deliver the same amount of medicine into your bloodstream as the brand. It’s not cheaper because it’s weaker-it’s cheaper because we’re no longer paying for the brand name.” Then add: “For drugs like yours, even small changes matter. That’s why we’ll check your blood levels in a week to make sure everything’s still on track.” This isn’t just a script. It’s a framework: acknowledge, explain, reassure, commit to monitoring.What to Say About Safety and Effectiveness
Avoid saying, “It’s the same thing.” That’s not true. Generics use different fillers, coatings, and manufacturing processes. But they’re therapeutically equivalent. That’s the key distinction. Use analogies. “Think of it like two different brands of aspirin. One’s Bayer, one’s store brand. Same active ingredient. Same effect. Just different packaging and price. For your medicine, we’ve checked that the amount of active drug in your bloodstream stays exactly where it needs to be.” Cite your own practice. “I prescribe this same generic to my own family. I wouldn’t give it to them if I didn’t trust it.” That’s powerful. People don’t trust data. They trust people.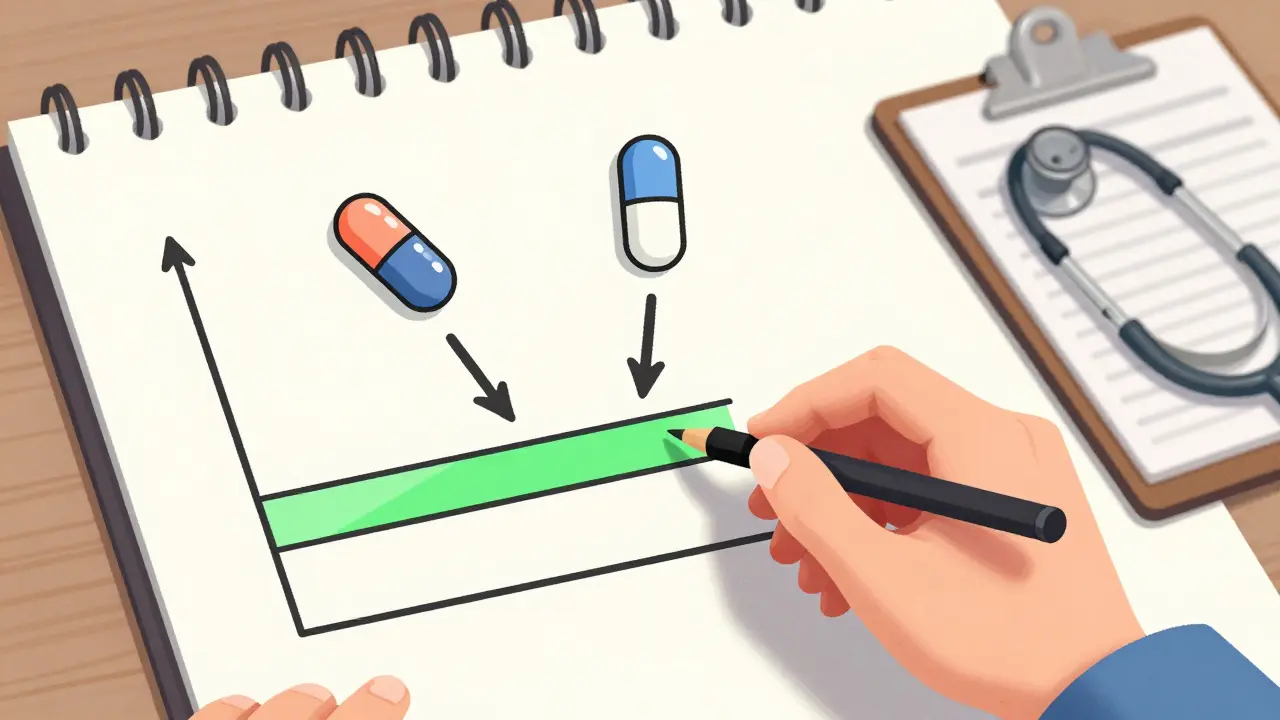
Monitoring Isn’t Optional-It’s the Core of the Plan
The FDA, the American Heart Association, and the American Epilepsy Society all agree: after switching an NTI drug, monitor early and often.- For warfarin: Check INR within 3-5 days.
- For levothyroxine: Check TSH in 6-8 weeks, but consider a baseline check at 2 weeks if the patient is elderly or has heart disease.
- For phenytoin or carbamazepine: Serum level check within 7-10 days.
State Laws Vary-Know Your Rules
In 27 U.S. states, pharmacists can’t switch an NTI drug without your explicit approval. Fourteen of those require written consent. In others, they can switch automatically-but you still need to inform the patient. Don’t assume your pharmacy is handling it. Confirm: “Did your pharmacist tell you about the switch? Did they give you a form to sign?” If not, you’re responsible for making sure the patient understands. This isn’t just clinical-it’s legal.Use Visuals. They Work.
A 2023 survey found that pharmacists who used simple charts or diagrams during counseling had 42% higher patient adherence. Show a line graph with the therapeutic range. Circle where their current level sits. Point to the generic’s expected range. Make it visual. People remember pictures better than words. Even a hand-drawn sketch on a notepad works. “Here’s your target zone. This is where we want you. The generic keeps you right here.”Special Populations Need Extra Care
Elderly patients? Those with kidney or liver problems? Those on five or more medications? These groups are at higher risk for NTI drug issues. Their bodies process drugs slower. Interactions are more likely. They’re more sensitive to small changes. For them, monitor sooner. Consider more frequent checks. Don’t wait for symptoms. Proactive monitoring prevents crises.
What to Do If Problems Arise
If a patient reports new symptoms-fatigue, dizziness, mood changes, unexplained bruising, or seizure activity-don’t dismiss it. Don’t assume it’s “just stress.” Check their medication history. Did they switch generics recently? Did they change pharmacies? Did they refill at a different location? These are red flags. Order a blood test. Even if the timing seems early. Better safe than sorry. If levels are off, switch back to the original brand. Not because the generic failed-but because the patient’s body reacted unpredictably. That’s not failure. That’s personalized medicine.The Bigger Picture
NTI generics are safe. The data proves it. But safety isn’t just about chemistry. It’s about trust. And trust is built through clear, consistent, compassionate communication. The FDA’s 2024 NTI Drug Communication Initiative gives providers standardized tools: counseling checklists, multilingual handouts, visual aids. Use them. Don’t reinvent the wheel. And remember: your goal isn’t to convince patients to accept generics. It’s to help them feel safe while they’re on them. When they know you’re watching, testing, and listening-they’ll trust you more than any label ever could.What to Document
Make sure your notes include:- “Patient counseled on therapeutic equivalence of generic [drug name] to brand version.”
- “Advised of need for [specific test] within [timeframe].”
- “Provided written educational materials.”
- “Patient verbalized understanding using teach-back method.”
Are generic NTI drugs really as safe as brand-name ones?
Yes-when they’re properly manufactured and monitored. The FDA requires stricter testing for NTI generics than for regular ones. For example, the blood levels of a generic warfarin must stay within 90-111% of the brand’s levels, not the usual 80-125%. Studies show that when patients are monitored after switching, outcomes are nearly identical to staying on the brand. But safety depends on follow-up. Without checking blood levels, even a safe drug can become risky.
Why do some patients have problems after switching to a generic NTI drug?
It’s rarely because the generic is faulty. More often, it’s because the patient wasn’t monitored after the switch. Small differences in absorption-maybe due to food, other meds, or even gut changes-can push blood levels out of range. Patients with kidney or liver issues, older adults, or those on multiple drugs are especially vulnerable. The problem isn’t the drug. It’s the lack of follow-up.
Can I switch back to the brand if the generic causes side effects?
Absolutely. If a patient reports new symptoms-like fatigue, confusion, or irregular heartbeat-after switching, check their blood levels. If they’re outside the target range, switching back to the original brand is a valid and common clinical decision. This isn’t admitting failure. It’s responding to individual needs. Some people’s bodies just respond better to one formulation over another, even if both are FDA-approved.
Do I need to get written consent from the patient before switching?
It depends on your state. Fourteen states require written patient consent before substituting an NTI drug. In others, verbal counseling is enough-but you still need to document it. Check your state’s pharmacy board rules. Even if not legally required, getting a signed acknowledgment is a smart practice. It shows you took the time to explain the change and the patient understood.
What if my patient refuses to switch to a generic?
Respect their choice. Forcing a switch without trust can backfire. Ask why they’re hesitant. Are they worried about cost? Side effects? Past bad experiences? Address the real concern. Offer to check their insurance coverage-sometimes the brand isn’t even more expensive. If they still refuse, keep them on the brand. You can revisit the conversation later, especially if costs become unmanageable. The goal is long-term adherence, not short-term savings.
How often should I check blood levels after switching?
For warfarin, check INR within 3-5 days. For phenytoin or carbamazepine, check serum levels within 7-10 days. For levothyroxine, check TSH in 6-8 weeks-but consider an early check (2-4 weeks) for older patients or those with heart conditions. Always follow your professional guidelines and the patient’s individual risk profile. Don’t wait for symptoms to appear-monitor proactively.
Are there any NTI drugs that shouldn’t be switched at all?
The FDA doesn’t say any NTI drug is off-limits for generics. But in practice, some patients-especially those with a history of instability after past switches, or those with complex medical conditions-do better staying on one formulation. If a patient has been stable for years on a brand, and switching offers no clear benefit (like lower cost or better access), it’s often wiser to leave them alone. Stability is a treatment goal in itself.
Next Steps for Providers
- Review your state’s NTI substitution laws. Know what’s required.
- Download the FDA’s 2024 NTI Counseling Toolkit. Use the checklists.
- Print out simple visual aids for common NTI drugs. Keep them in your exam room.
- Train your staff. Nurses and pharmacists should know the key messages too.
- Document every counseling session. Use consistent language.



Let me tell you something-this whole generic NTI thing is a corporate scam wrapped in FDA paperwork. I’ve seen patients crash after switching. One guy went from stable INR of 2.4 to 4.8 in three days. They call it ‘therapeutic equivalence’? More like therapeutic roulette. The FDA doesn’t test for long-term effects, only peak absorption. And don’t even get me started on fillers-some generics use lactose, gluten, dyes… stuff that can trigger immune responses in sensitive people. This isn’t science. It’s profit-driven negligence.