Imagine you’re on a medication that’s been working fine for months. Then you see a headline: "FDA issues safety alert for common blood pressure drug." Your heart skips. Is this something you need to worry about? Should you stop taking it? Who do you even ask?
You’re not alone. Every year, the FDA issues hundreds of drug safety alerts-warnings about new risks tied to medications you’re already taking. But here’s the problem: most patients don’t know how to bring these up with their doctor without sounding alarmist, confused, or even paranoid. And doctors? They’re drowning in alerts themselves. The key isn’t just knowing the alert exists-it’s knowing how to talk about it in a way that gets results.
What Exactly Is a Drug Safety Alert?
A drug safety alert isn’t a rumor. It’s a formal notice from the U.S. Food and Drug Administration (FDA) about a newly discovered risk linked to a medication. These aren’t random blog posts or Facebook memes. They’re based on real data-from thousands of patient reports, clinical studies, and long-term monitoring systems like MedWatch.
These alerts can mean anything from a rare but serious side effect-like liver damage or heart rhythm problems-to something more common, like a dosage change or a warning that the drug shouldn’t be mixed with another medication you’re taking. In 2023 alone, the FDA issued alerts about stimulants for ADHD, opioid painkillers, and even Alzheimer’s drugs like Leqembi, requiring new MRI monitoring rules.
Not every alert applies to you. That’s the catch. An alert might say, “Risk increases in patients over 70 with kidney disease.” If you’re 45 and your kidneys are fine, the alert doesn’t change your plan. But if you fit the profile? That’s when you need to talk to your doctor.
Why Most Patients Get It Wrong
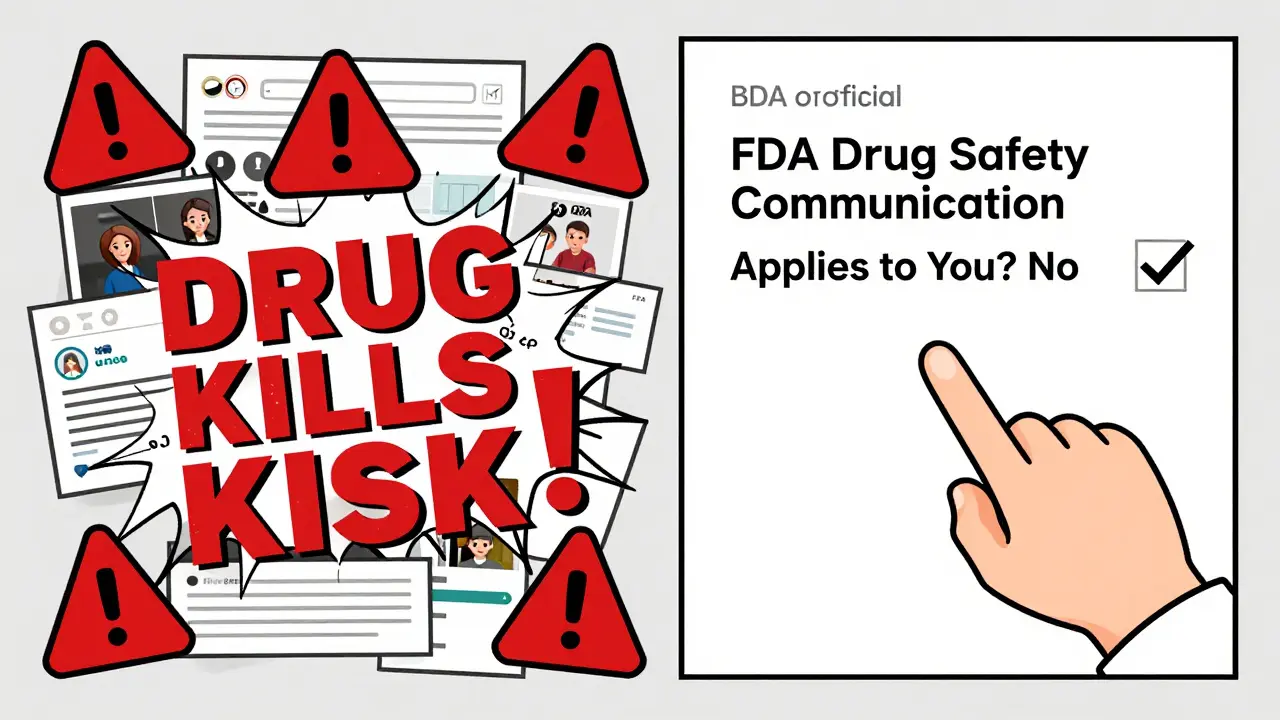
Too many people walk into an appointment with a printed-out news article or a screenshot from Twitter. They say, “This drug is dangerous!” and expect the doctor to panic.
That doesn’t work. Doctors hear this all the time-and they’ve seen how misinformation spreads. A Mayo Clinic review found that patients who brought in FDA’s official Drug Safety Communication (the real document, not a summary) were taken seriously 80% of the time. Those who brought in social media posts? Often dismissed.
Here’s the truth: your doctor isn’t ignoring you. They’re overwhelmed. A 2021 study showed only 37% of primary care doctors regularly check for new safety updates between visits. So when you show up with a well-prepared question, you’re not just asking for help-you’re helping them do their job better.
How to Find the Real Alert (Not the Noise)
Start at the source: fda.gov/drugs/drug-safety. Type in your medication’s name. Look for the official Drug Safety Communication. It will have a date, a clear summary, and a link to the full report.
Don’t trust headlines. Read the whole thing. Alerts often say things like, “Risk is increased only in patients with X condition,” or “Monitor liver enzymes every 3 months.” That’s the info you need.
Print it. Or save the PDF. Don’t rely on your phone screen. Doctors appreciate it when you come prepared with the actual document. It shows you’ve done your homework-and you’re not just reacting to fear.
What to Say (and Not Say) at Your Appointment
Here’s the script that works: “I saw this FDA safety alert about [medication name], dated [date]. I wanted to talk about whether it applies to me.”
That’s it. No yelling. No accusations. Just facts and curiosity.
Don’t say:
- “This drug is going to kill me!”
- “Why didn’t you tell me about this?”
- “I read online that everyone should stop taking it.”
Do say:
- “Does this new warning change how we should monitor my health?”
- “Are there alternatives if this becomes risky for me?”
- “Should I get any new tests because of this?”
Timing matters too. Bring it up in the first two or three minutes of your appointment. That’s when your doctor’s attention is sharpest. Waiting until the end? You might get a rushed “We’ll talk next time.” And next time might never come.
What Your Doctor Might Say-and How to Respond
Most doctors (about 68% of them, according to patient surveys) will welcome the discussion. They’ll say things like:
- “That’s a good catch. This alert doesn’t apply to you because you don’t have [condition].”
- “We’re already monitoring for that. Your last blood test was normal.”
- “Let’s switch you to a different medication just to be safe.”
But sometimes, you’ll get the opposite:
- “That’s just alarmist.”
- “We’ve been using this drug for decades.”
- “I don’t pay attention to those alerts.”
If that happens, don’t argue. Say: “I understand you’ve seen this before. But since the FDA updated their warning, could we at least check my [blood work, kidney function, heart rhythm] to be sure?”
That shifts the conversation from disagreement to collaboration. And it gives you a clear next step.
What If You’re on Multiple Medications?
Most people aren’t on just one drug. The average patient over 65 takes five or more. That’s where things get complicated. An alert might say, “Don’t take this with drug X.” But what if you’re also on drug Y and Z? That interaction might not be listed.
Bring your full list-every pill, every patch, every supplement-to your appointment. Even the herbal ones. The FDA alert might not mention interactions with St. John’s Wort or grapefruit juice, but your doctor needs to know.
Pharmacovigilance systems (that’s the fancy term for drug safety tracking) struggle with polypharmacy. So you’re the missing piece. You know what you’re taking. Your doctor doesn’t. Help them connect the dots.
What Happens After the Conversation?
Good conversations lead to action. You might get:
- A new lab test scheduled
- A dosage adjustment
- A switch to a different medication
- Or, reassuringly, confirmation that nothing needs to change
Either way, get it in writing. Ask your doctor to note the discussion in your chart. If they say, “We’ll just keep an eye on it,” ask: “What are we watching for? And when should I come back?”
Also, sign up for FDA email alerts. You can choose to get updates for specific drugs or categories-like “blood pressure meds” or “antidepressants.” That way, you’re not scrambling every time you hear a headline.
When to Seek a Second Opinion
If your doctor dismisses a serious alert-like one tied to heart failure, liver damage, or suicidal thoughts-and you feel unheard, it’s okay to get another opinion. Don’t wait. Go to a pharmacist, a specialist, or another primary care provider. Bring your documents. Say: “I was told this isn’t a concern, but I’m worried.”
Medication safety isn’t about being paranoid. It’s about being informed. The FDA doesn’t issue alerts lightly. They’re based on real harm-sometimes hundreds of cases. Your doctor might not see every alert, but you can be the one who does.
Final Tip: Keep a Medication Log
Start a simple notebook or phone note with:
- Medication name
- Dosage
- Why you’re taking it
- Date of last safety alert check
- Doctor’s response
Update it every time you talk to your doctor. In six months, you’ll have a clear record of your care-and if something goes wrong, you’ll have proof you were proactive.
Drug safety isn’t just the FDA’s job. It’s yours too. You’re the one taking the pill. You’re the one noticing side effects. You’re the one who knows your body best. Use that power wisely.



Bro, I just printed the FDA alert for my blood pressure med and handed it to my doc like a boss. He actually paused and said, "Wow, you read the whole thing?" I nodded. He changed my dosage next week. Stop scrolling. Start printing.