Methadone QT Risk Calculator
Risk Assessment Tool
Enter your specific details to assess your risk of QT prolongation while taking methadone.
When someone starts methadone for opioid dependence or chronic pain, they’re often told to take it once a day. It’s effective. It’s affordable. But few patients are warned about what happens behind the scenes in their liver - and how that can quietly put their heart at risk.
How Methadone Changes Your Heart’s Rhythm
Methadone doesn’t just block pain signals or reduce cravings. It also blocks a specific ion channel in heart cells called hERG. This slows down the electrical reset between heartbeats, which shows up on an ECG as a longer QT interval. A normal QTc (corrected for heart rate) is under 430 milliseconds for men and under 450 for women. Once it hits 470, the risk starts climbing. At 500 or higher, the chance of sudden cardiac death jumps fourfold. In one study of 167 methadone patients, nearly 30% had QTc intervals over 460 ms - more than triple the rate in people not taking methadone. And in 16% of those patients, the QTc reached 500 ms or more. That’s not rare. That’s common enough that clinics should be checking ECGs before and during treatment.Why CYP Enzymes Are the Hidden Trigger
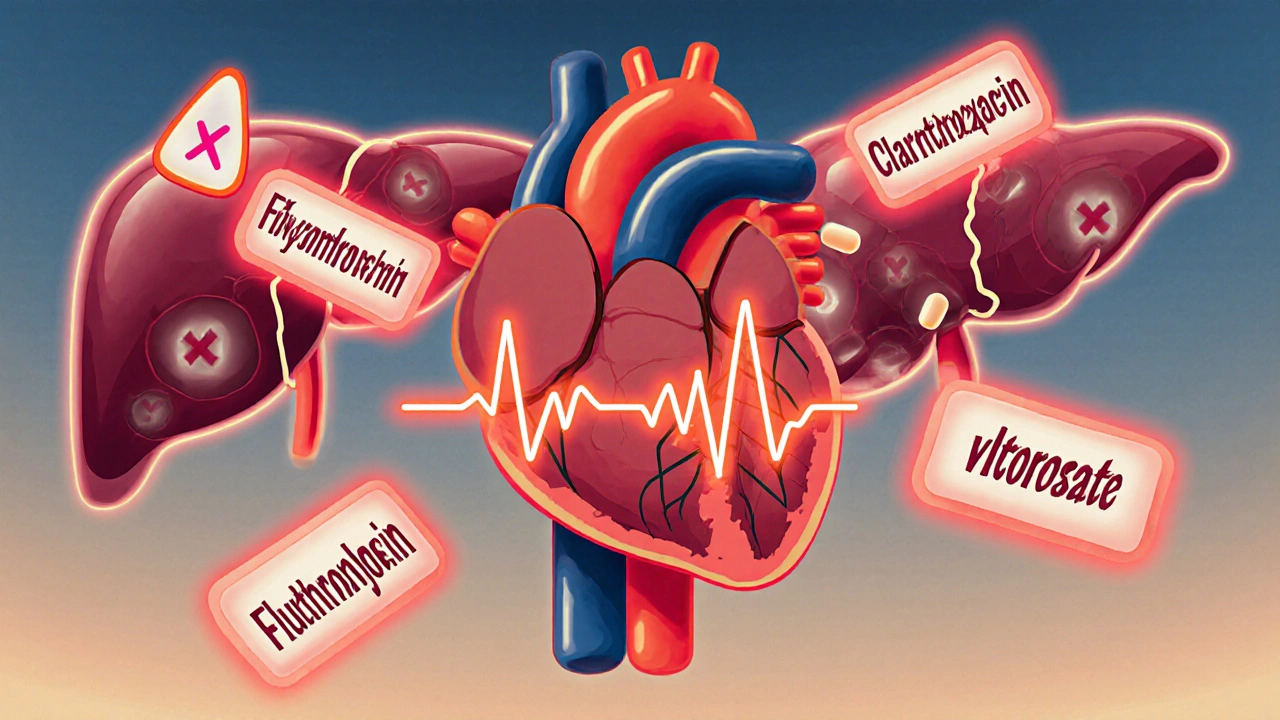
Methadone is broken down mostly by two liver enzymes: CYP3A4 and CYP2B6. When something blocks these enzymes - like a common antibiotic, antifungal, or antidepressant - methadone doesn’t get cleared. It builds up. And with higher levels in the blood, the heart-blocking effect gets stronger. The biggest culprits? Fluoxetine (Prozac), clarithromycin (Biaxin), fluconazole (Diflucan), and valproate (Depakote). In the same 2007 study, these drugs showed up in nearly half the patients with dangerous QT prolongation. One patient taking methadone and fluoxetine had a QTc jump from 420 to 510 ms in just two weeks. No dose change. Just the added drug. Even worse, methadone itself can inhibit CYP enzymes. So it’s not just other drugs affecting methadone - methadone can also interfere with how other drugs are processed. This creates a tangled web of interactions that’s hard to predict.Dose Doesn’t Tell the Whole Story
You’d think higher doses mean higher risk. And sometimes, yes. Doses above 100 mg/day are linked to more QT prolongation. But here’s the problem: some people on 40 mg have dangerous QT prolongation, while others on 200 mg never do. A review of 32 cases of methadone-related torsade de pointes (a dangerous heart rhythm) found that only 21 showed a clear link to dose. The rest? Their risk came from something else - like low potassium, heart disease, or a hidden drug interaction. This is why doctors can’t rely on dose alone. Two people on the same dose, with the same weight and history, can have wildly different outcomes. One might be fine. The other could collapse without warning.
Who’s Most at Risk?
The people most likely to have a bad reaction to methadone share a few traits:- Taking a CYP3A4 or CYP2B6 inhibitor (fluoxetine, clarithromycin, ritonavir, etc.)
- Low potassium or magnesium levels
- Existing heart disease or history of arrhythmias
- Female gender (women naturally have longer QT intervals)
- Older age or liver problems
- Using other QT-prolonging drugs (some antipsychotics, anti-nausea meds, or even certain antibiotics)
What Clinicians Are Doing About It
Back in 2009, San Mateo County Health started requiring ECGs for anyone on methadone doses of 100 mg or more. That made sense - higher dose, higher risk. But new data changed that. In 2023, the American Society of Addiction Medicine updated its guidelines. Now, they recommend baseline ECGs for anyone starting methadone at 50 mg or higher. Why? Because studies found QT prolongation happening even at lower doses - especially when CYP inhibitors were involved. The protocol is simple:- Get a baseline ECG before starting methadone.
- Repeat it after 1-2 weeks, once the dose is stable.
- Check again if the dose is increased, or if a new medication is added.
- Monitor electrolytes - especially potassium - every 1-3 months.
- Use a drug interaction checker before prescribing anything new.
What to Avoid - The Top 5 Dangerous Combinations
These five drugs are the most common triggers for dangerous methadone interactions:- Fluoxetine (Prozac, Sarafem) - a strong CYP2D6 and CYP3A4 inhibitor
- Clarithromycin (Biaxin) - a potent CYP3A4 blocker
- Fluconazole (Diflucan) - inhibits CYP2C9 and CYP3A4
- Valproate (Depakote) - reduces methadone clearance
- Ritonavir (in Paxlovid) - a powerful CYP3A4 inhibitor, now commonly used for COVID-19

Buprenorphine: The Safer Alternative?
Many patients and providers are turning to buprenorphine because it’s just as effective for cravings - but doesn’t prolong the QT interval. Studies show buprenorphine has minimal effect on heart rhythm, even at high doses. In 2021, buprenorphine prescriptions in the U.S. hit 2.1 million - up from 1.4 million in 2016. Methadone is still used more overall, but buprenorphine’s share is growing fast. For patients with existing heart conditions, older adults, or those on multiple meds, buprenorphine is often the smarter first choice.What Patients Should Know
If you’re on methadone, here’s what you need to do:- Ask for an ECG before you start - and after any dose change.
- Keep a list of every medication, supplement, or herb you take - including over-the-counter stuff.
- Don’t start any new drug without checking with your prescriber.
- Know the signs of dangerous heart rhythm: dizziness, fainting, palpitations, shortness of breath.
- Get your potassium checked regularly - especially if you’re on diuretics or have vomiting/diarrhea.
The Bigger Picture
Methadone saves lives. But it’s not a safe drug. It’s a powerful one - and it demands respect. The 390% rise in methadone-related deaths between 1999 and 2004 wasn’t because people were taking too much. It was because no one was checking their hearts. Today, we have the tools: ECGs, drug interaction checkers, potassium tests, and clearer guidelines. But they’re only useful if they’re used. Clinics that skip ECGs are gambling with patient lives. Patients who don’t speak up about their meds are putting themselves at risk. And doctors who don’t ask about all the pills - including those bought online or prescribed by other providers - are missing the full picture. The science is clear. The protocols exist. The question isn’t whether methadone is dangerous. It’s whether we’re willing to do what it takes to keep people safe while using it.Can methadone cause sudden cardiac death even at low doses?
Yes. While higher doses increase risk, methadone has caused fatal heart rhythms in patients taking as little as 30-50 mg per day - especially when combined with CYP inhibitors like fluoxetine or fluconazole. The interaction matters more than the dose alone.
How long does methadone stay in the body, and why does that matter for QT risk?
Methadone has a half-life of 8 to 59 hours, meaning it can stay in your system for several days. This means QT prolongation can persist even after you stop a drug that interacts with it. If you take clarithromycin for 7 days and then stop, your methadone levels may still be elevated for another week - and your heart remains at risk.
Should I get an ECG if I’m on less than 50 mg of methadone?
If you have other risk factors - like low potassium, heart disease, or you’re taking any other QT-prolonging drug - then yes. Even at low doses, interactions can push your QT interval into the danger zone. The 50 mg guideline is a starting point, not a safety cutoff.
Can I switch from methadone to buprenorphine safely?
Yes, but it must be done carefully under medical supervision. Switching too quickly can trigger withdrawal. Most protocols involve gradually reducing methadone while introducing buprenorphine, with close monitoring for withdrawal symptoms and cardiac stability. Buprenorphine is a safer long-term option for those with heart risks.
What should I do if I feel dizzy or faint while on methadone?
Stop what you’re doing and sit or lie down. Call your provider immediately. These can be early signs of torsade de pointes, a life-threatening arrhythmia. Do not wait. Get an ECG as soon as possible. Do not drive or operate machinery until cleared by a doctor.
Are there any blood tests that can predict methadone-related QT risk?
Not yet. While genetic tests for CYP2B6 variants are being studied, they’re not routine. The best predictors are still clinical: ECGs, drug lists, electrolyte levels, and heart history. No blood test can replace an ECG when it comes to assessing QT risk.


I had no idea methadone could mess with your heart like this. I’ve been on it for 3 years at 60mg and never thought to ask for an ECG. My doctor just said 'take it daily' and left it at that. Scary stuff.