Obesity Medication Dosing Calculator
Calculate Your Adjusted Body Weight
Medication Dosing Recommendations
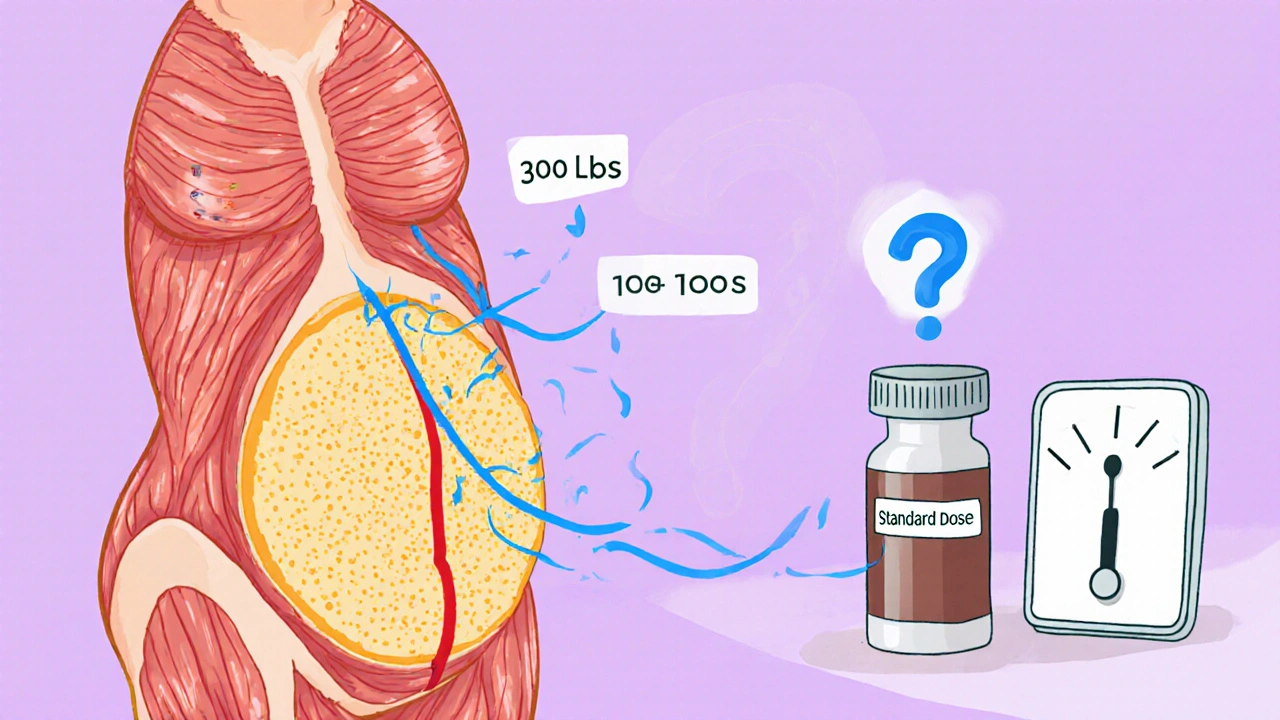
When you’re overweight or obese, your body doesn’t just carry extra weight-it changes how medicines work. A 300-pound person doesn’t need three times the dose of a 100-pound person. In fact, giving more just because someone weighs more can be dangerous. Too little, and the drug won’t work. Too much, and it can cause serious side effects. This isn’t guesswork. It’s science. And it’s happening every day in hospitals, clinics, and pharmacies around the world.
Why Standard Dosing Fails in Obesity
Most drug labels still list doses based on average body weight. But that average doesn’t include people with obesity. In the U.S., nearly 40% of adults have a BMI over 30. Globally, obesity rates have more than doubled since 1990. Yet, only 18% of drug labels give any guidance for obese patients. That leaves doctors and pharmacists to figure it out on their own-and too often, they get it wrong. The problem starts with how drugs move through the body. Some drugs dissolve in fat (lipophilic), others in water (hydrophilic). In obesity, fat tissue expands. That changes where the drug goes and how long it stays. For example, diazepam, a sedative, spreads into fat. In someone with severe obesity, its volume of distribution jumps from 1.1 L/kg to 2.8 L/kg. If you give the same dose as a normal-weight person, the drug gets diluted too much. It won’t work. On the flip side, antibiotics like cephazolin are water-soluble. They stay in blood and tissues with good blood flow. But in obesity, blood volume and kidney function increase. The drug gets cleared faster. A standard 1g dose for surgery prophylaxis often leads to subtherapeutic levels. Studies show that 58% of obese patients on standard doses don’t reach the minimum concentration needed to kill bacteria. That means higher infection rates after surgery.Lean Body Weight vs. Total Body Weight: What’s the Difference?
Doctors now use three main ways to calculate doses for obese patients:- Total Body Weight (TBW): Your actual weight on the scale. Often too high for water-soluble drugs, too low for fat-soluble ones.
- Ideal Body Weight (IBW): The weight you’d have if you had normal body fat. For men: 50 kg + 2.3 kg for every inch over 5 feet. For women: 45.5 kg + 2.3 kg per inch over 5 feet.
- Adjusted Body Weight (AdjBW): A middle ground. Formula: IBW + 0.4 × (TBW − IBW). This accounts for extra weight without overestimating.
- BMI 40-49.9: 40 mg twice daily
- BMI ≥50: 60 mg twice daily
Antimicrobials: Where the Rules Are Clearest
Antibiotics are the most studied class in obesity dosing. That’s because failure means death-sepsis, surgical infections, prolonged hospital stays. Take vancomycin. It’s used for MRSA. If levels are too low, the infection won’t clear. Too high, and it can wreck your kidneys. Stanford’s 2022 study found that when dosed by total body weight, 39% of obese patients had toxic levels. When they switched to AdjBW, that dropped to 12%. Their electronic alert system cut subtherapeutic levels from 31% to 9%-and shortened hospital stays by over two days. Colistin is another example. It’s toxic to kidneys. The Infectious Diseases Society of America (IDSA) recommends capping daily dose at 360 mg colistin base activity (CBA) or 12 million units, based on IBW. Why? Because in obese patients, 44% develop kidney damage with standard dosing, compared to 29% in normal-weight people. Tigecycline is different. Dosing doesn’t change with weight. The standard is 100 mg loading dose, then 50 mg every 12 hours. But a 2024 update suggests doubling the dose (200 mg loading, 100 mg maintenance) for resistant infections-regardless of BMI. That’s because the drug’s effectiveness doesn’t improve with higher doses in obese patients; it just increases side effects like nausea and vomiting.
Other Drugs with Critical Dosing Differences
Not all medications are antibiotics. Many common ones need special handling. Apixaban, a blood thinner, has a dangerous cliff edge. It’s dosed at 5 mg twice daily for people under 85 kg, and 10 mg for those 85 kg or heavier. That’s a 100% jump at one number. Medicare data shows people just above 85 kg have a 47% higher risk of bleeding than those just below. There’s no gradual increase. Just a sudden, risky leap. Carvedilol, a beta-blocker, uses the same binary system. 50 mg daily if under 85 kg. 100 mg if 85 kg or over. But metoprolol uses a continuous scale: 5 mg per kg of body weight, up to 200 kg. That smooth curve avoids the dangerous spikes and drops you see with dichotomized dosing. Voriconazole, an antifungal, is another case where total body weight causes toxicity. When dosed by TBW, 39% of obese patients get too much. Using AdjBW cuts that to 12%. That’s why Stanford Health Care now requires therapeutic drug monitoring (TDM) for all obese patients on voriconazole.Therapeutic Drug Monitoring: The Missing Piece
The best way to know if a dose is right? Measure it. That’s therapeutic drug monitoring (TDM). It’s not optional anymore for many drugs in obese patients. IDSA guidelines strongly recommend TDM for vancomycin, aminoglycosides, and voriconazole in patients with BMI over 30. Yet, only 37% of U.S. hospitals have formal obesity dosing protocols. And only 63% of pharmacists say their institutions support TDM programs. Why the gap? Cost. Time. Lack of training. TDM requires blood draws, lab analysis, and someone to interpret results. But the cost of getting it wrong-readmissions, kidney failure, surgical infections-is far higher. At Mayo Clinic, implementing TDM for vancomycin reduced subtherapeutic levels by 71% and cut hospital stays by 2.3 days. That’s not just better care. It’s cheaper care.
What’s Holding Back Better Dosing?
The science is clear. The guidelines exist. So why do 68% of hospital pharmacists still report dosing errors in obese patients? One big reason: confusion over which weight to use. A 2021 University of Michigan study found 43% of internal medicine residents didn’t know when to use IBW vs. TBW. One patient with BMI 52 got too much heparin. She developed heparin-induced thrombocytopenia-a life-threatening drop in platelets. Another problem: outdated drug labels. The FDA only requires obesity-specific data in new drug trials since 2021. Even then, only 22% of new drug applications in 2022-2023 included enough data on obese patients. Most labels still say “use standard dose.” And training? Most pharmacists need 6-8 hours of specialized education to get 90% accuracy on AdjBW calculations. Standard dosing? Two hours. That’s a huge barrier in fast-paced clinics.What’s Changing-and What’s Coming
Change is happening, slowly. The FDA’s March 2024 draft guidance now requires obesity subgroup analysis for patients with BMI over 50. That’s a big step. Before, only 4% of trials included people with BMI above 45. The NIH just awarded $4.7 million to the University of Pittsburgh to track 500 obese patients over five years. They’re studying how drug handling changes across age, sex, and fat distribution. And tools are getting smarter. DoseMe, an Australian company, offers Bayesian TDM software used by 83% of U.S. academic medical centers. It adjusts doses in real time based on blood levels, weight, kidney function, and more. In the next five years, experts predict we’ll combine body composition scans with genetic testing. Imagine knowing not just your BMI, but your muscle-to-fat ratio, liver enzyme activity, and how your genes process drugs. That’s the future of precision dosing.What You Can Do Right Now
If you or someone you care for has obesity and takes medication:- Ask: “Is this dose based on my actual weight, or should it be adjusted?”
- Ask: “Do I need a blood test to check if the drug level is right?”
- Keep a record of your weight and BMI. If you’ve lost or gained weight, tell your doctor.
- Use reliable tools like the Clincalc Obesity Dosing Reference (updated weekly) to check common drugs.


Okay, so I just spent 45 minutes reading this and honestly? My brain is full. Like, I didn’t realize that diazepam just... disappears into fat tissue? And that cephazolin gets flushed out so fast in obese patients that it’s basically useless? I’ve had two surgeries in the last three years and I’m 290 lbs-no one ever told me any of this. I just assumed they knew what they were doing. Now I’m scared to take anything. Also, AdjBW? I had to Google that three times. Can we get a cheat sheet? Like, a printable PDF? I’d print 12 copies and tape them to my fridge, my bathroom mirror, my cat’s collar. 🤯