Itching from opioids isn’t always an allergy - here’s how to tell the difference
If you’ve ever taken morphine or oxycodone and broke out in a rash or couldn’t stop scratching, you’re not alone. Most people assume it’s an allergy. But here’s the truth: itching from opioids is rarely a true allergic reaction. In fact, up to 80% of patients labeled "allergic" to opioids are actually experiencing a harmless, predictable side effect called a pseudoallergic reaction. The confusion isn’t your fault - it’s been baked into medical records for decades. But misunderstanding this distinction can cost you better pain control, more medication options, and even higher bills.
True opioid allergies are rare. They involve your immune system attacking the drug like a foreign invader. Symptoms? Swelling of the lips or throat, trouble breathing, a sudden drop in blood pressure, or a widespread, blistering rash. These reactions happen fast - often within minutes - and can be life-threatening. But if your only symptom is itching, flushing, or mild nausea? That’s almost certainly not your immune system. It’s your mast cells releasing histamine directly, no antibodies involved. Think of it like a false alarm: your body reacts, but it’s not actually allergic.
Why morphine makes you itch - and why fentanyl doesn’t
Not all opioids are created equal when it comes to itching. Morphine is the worst offender. It triggers histamine release from mast cells in your skin at very low doses - as little as 0.1 mg per kilogram of body weight. That’s why patients often say, "I got itchy right after my first IV morphine dose." Codeine does the same thing. But fentanyl? Almost none. Methadone? Very little. Why? It’s chemistry. Morphine has a specific molecular shape - a tertiary amine group - that acts like a key turning a lock on mast cells, forcing them to dump histamine. Fentanyl and methadone lack that key. They slide right past.
That’s why switching opioids can be the simplest fix. If morphine makes you itch, try fentanyl. A 2019 study found that switching from morphine or oxycodone to fentanyl cut itching rates from 30-40% down to 10-15%. Even better, methadone causes itching in only 5-10% of patients. And here’s the kicker: you don’t have to sacrifice pain relief. These alternatives are just as effective - they just don’t trigger the same histamine flood.
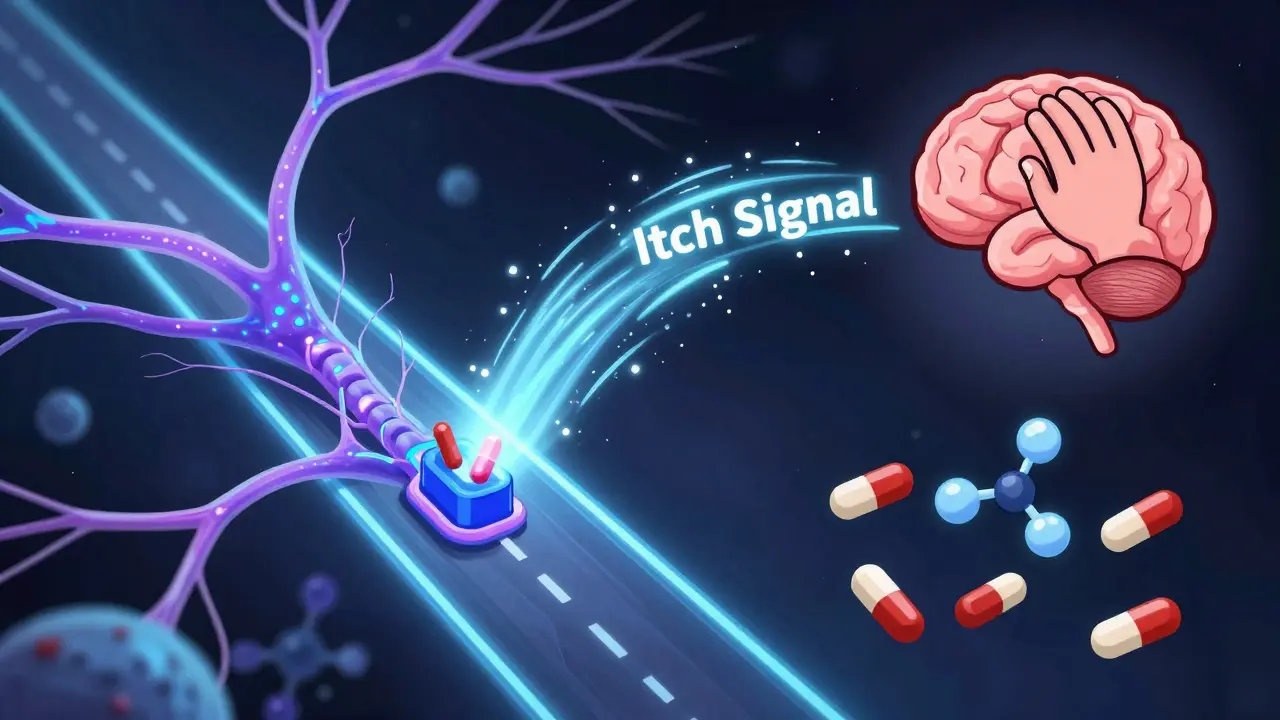
Itching isn’t just histamine - your spine is involved too
Here’s where it gets even more interesting. Not all opioid-induced itching comes from histamine. In fact, some of it starts in your spinal cord. Researchers at Washington University discovered in 2007 that opioids activate a specific receptor in the spine called GRPR - gastrin-releasing peptide receptor. When this receptor fires, it sends a signal that your brain interprets as itch, even if your skin is perfectly normal. This explains why antihistamines like Benadryl sometimes don’t work. You’re treating the wrong part of the chain. That’s why newer drugs like nalfurafine - approved in Japan and now in late-stage U.S. trials - target this spinal pathway directly. They reduce itching by 70% without dulling pain. This isn’t science fiction. It’s coming to clinics soon.
What to do when you get itchy - step by step
Don’t panic. Don’t stop your medication. Don’t label yourself "allergic" unless you’re sure.
- Step 1: Assess the symptoms. Is it just itching? Flushing? Mild dizziness? That’s likely pseudoallergic. If you have swelling, wheezing, or a drop in blood pressure - call for help immediately.
- Step 2: Talk to your doctor. Don’t assume it’s an allergy. Ask: "Could this be a histamine reaction?" Show them your symptoms and when they started.
- Step 3: Try a lower dose. Reduce your opioid dose by 25-50%. Often, itching fades as your body adjusts.
- Step 4: Add an antihistamine. Take diphenhydramine (Benadryl) 25-50 mg 30 minutes before your next opioid dose. It works in 80-90% of cases.
- Step 5: Switch opioids if needed. If itching persists, ask about fentanyl or methadone. Both have far lower histamine-releasing potential.
For cancer patients or those in palliative care, this approach is standard. A Harvard study found that 78% of patients with "opioid allergy" labels tolerated a different opioid after using antihistamines. Only 5% had true allergic reactions.
Why mislabeling opioids as allergies is dangerous
Here’s the real cost: when you’re labeled "allergic to opioids," doctors avoid giving you anything effective. They turn to weaker painkillers, non-opioid combos, or even avoid treatment altogether. The result? More suffering. More ER visits. More unnecessary procedures.
A 2020 study in JAMA Internal Medicine found that mislabeled opioid allergies cost the U.S. healthcare system $1,200 per patient - mostly because of pricier, less effective alternatives. Multiply that by 20-30 million opioid users annually, and you’re looking at $24-36 billion wasted. And it’s not just money. Patients miss out on better pain control, faster recovery, and improved quality of life.
Worse, many patients self-label. A 2023 survey found 68% of oxycodone users got itchy - but only 12% told their doctor. Most just took OTC antihistamines and kept going. That’s why 87% of people who say they’re "allergic to opioids" actually just had itching or nausea - side effects, not allergies.

When you really do have an opioid allergy - and what to do
True opioid allergies are rare - about 0.1-0.3% of exposures - but they’re serious. If you’ve ever had swelling of the tongue, trouble breathing, or passed out after an opioid, you need to be evaluated properly. You should avoid all opioids in the same chemical family (like morphine, codeine, oxycodone). But here’s the good news: fentanyl and methadone rarely cross-react. In fact, studies show cross-reactivity is less than 5%.
If you absolutely need an opioid - say, for surgery or cancer pain - desensitization is an option. It’s a controlled process where you get tiny, increasing doses of the drug over 4-6 hours under close monitoring. Success rates? Over 95%. It’s not common, but it’s life-changing for those who need it.
What’s next? Better tools, better care
Hospitals are finally catching on. Epic Systems, one of the biggest electronic health record platforms, added a feature in 2021 that lets clinicians tag reactions as "itching" or "true allergy" - not just "opioid allergy." That cut mislabeling by 45% across 1,200 hospitals.
And research is moving fast. Scientists are studying genetic markers that predict who’s likely to get histamine-driven itching. A simple blood test might one day tell you if you’re at high risk before you even take your first dose.
For now, the best tool you have is knowledge. Don’t let a simple itch keep you from the pain relief you need. Talk to your provider. Ask questions. Know the difference. You’re not allergic because you’re itchy. You’re itchy because of how the drug works. And that’s something you can fix - without giving up pain control.
Frequently Asked Questions
Is itching from opioids a sign of an allergy?
No, itching alone is almost never a true allergy. It’s a pseudoallergic reaction caused by histamine release from mast cells. True allergies involve swelling, trouble breathing, low blood pressure, or a widespread rash. If itching is your only symptom, it’s a side effect - not an allergy.
Can I still take opioids if I get itchy?
Yes, absolutely. You can reduce the dose, take an antihistamine like diphenhydramine before dosing, or switch to an opioid with lower histamine-releasing potential - like fentanyl or methadone. Most people who get itchy on morphine do fine on these alternatives.
Why doesn’t Benadryl always stop the itching?
Because not all opioid itching comes from histamine. Some of it is triggered by receptors in your spinal cord (GRPR), which antihistamines can’t touch. That’s why some patients still itch even after taking Benadryl. Newer drugs like nalfurafine target this spinal pathway and are much more effective.
Which opioids are least likely to cause itching?
Fentanyl and methadone cause the least itching - only 5-10% of users report it. Morphine and codeine are the worst offenders, with 30-40% of users getting itchy. Hydromorphone is in the middle - less histamine release than morphine but more than fentanyl.
Should I get skin tested for opioid allergy?
Usually not. Skin testing for opioids has a high false-positive rate - up to 30% - and doesn’t reliably predict real allergic reactions. Experts recommend avoiding it unless you had a life-threatening reaction like anaphylaxis. Instead, a supervised trial with a different opioid is safer and more accurate.
Can opioid itching lead to long-term problems?
Not directly. The itching itself is temporary and harmless. But if you’re mislabeled as "allergic," you may be denied effective pain treatment, leading to chronic pain, anxiety, or unnecessary procedures. The real risk isn’t the itch - it’s the label.


I used to get itchy as hell on morphine. Thought I was allergic till my pain doc explained the histamine thing. Benadryl before the dose? Game changer. No more avoiding pain meds just because my skin felt weird.
People need to stop self-diagnosing opioid allergies. It’s not helping anyone.