Pregnancy Back Pain Relief Finder
Find the right relief for your back pain
Answer a few questions to get personalized recommendations for safe, pregnancy-friendly back pain relief.
Your Back Pain Relief Recommendations
About This Tool
This tool recommends safe, pregnancy-friendly back pain relief options based on current medical guidelines. Always consult your healthcare provider before trying new treatments during pregnancy.
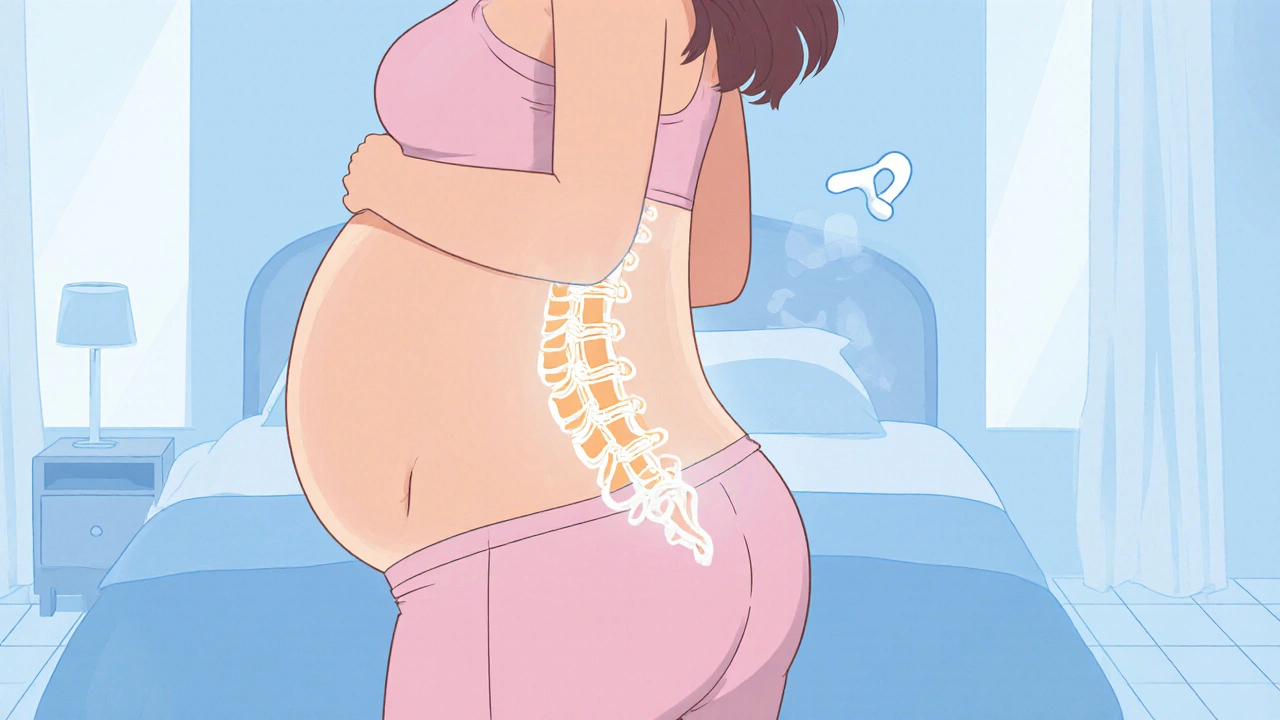
When a backache in pregnancy is a common discomfort caused by the many physical changes a body undergoes during gestation shows up, it can feel like a relentless ache that refuses to quit. You’re not alone-up to 70% of pregnant people report some sort of back trouble, and the good news is most of it can be managed safely at home.
Quick Takeaways
- Back pain in pregnancy is usually due to hormonal shifts, added weight, and altered posture.
- Gentle movement, supportive gear, and heat/cold therapy are the safest first‑line remedies.
- Avoid heavy lifting, prolonged standing, and any stretch that feels sharp.
- Seek medical help if pain is sudden, severe, or accompanied by fever, numbness, or urinary changes.
- Regular check‑ins with your obstetrician or a physical therapist keep you on track.
Why Does My Back Hurt When I’m Expecting?
Three big forces pull at your spine once the baby starts growing:
- Hormonal changes - The hormone relaxin loosens ligaments to ready the pelvis for birth. Unfortunately, those same ligaments also become lax around the lower back, reducing stability.
- Weight gain - The average gain of 25-35 kg adds a forward‑tilt to the pelvis, forcing the lumbar curve to over‑extend (hyperlordosis). That extra curve compresses the discs and muscles.
- Postural strain - As the belly expands, many people unconsciously sway forward, putting the upper back and neck in a hunched position.
Think of your spine as a flexible column. When the base starts wobbling, the whole structure strains to compensate, and the muscles scream for relief.
Risk Factors That Can Make Pain Worse
Not everyone experiences the same intensity. Certain factors raise the odds of a painful episode:
- Previous low‑back injuries or chronic back conditions.
- Carrying twins or a larger‑than‑average baby.
- Physically demanding jobs that require heavy lifting or prolonged standing.
- Pre‑existing scoliosis or pelvic asymmetry.
If any of these apply to you, you might want to start a gentle prevention plan early in the second trimester.

Safe Relief Tips You Can Try Today
Below is a quick‑reference table that sums up the most pregnancy‑friendly options. Each method is rated for comfort, ease of use, and safety level.
| Method | How It Helps | Pros | Cons / cautions |
|---|---|---|---|
| Heat therapy (warm compress) | Boosts blood flow, relaxes tightened muscles | Easy, inexpensive, can be applied while sitting | Don’t use >20 min at a time; avoid if you have swelling |
| Cold therapy (ice pack) | Reduces inflammation after a sudden strain | Quick relief for sharp aches | Wrap in cloth; limit to 15 min to avoid skin frostbite |
| Support belt | Provides external stability for the lumbar region | Wear during daily activities or long walks | Should not be too tight; remove for sleeping |
| Prenatal yoga / gentle stretching | Improves flexibility, strengthens core muscles | Can be done at home; many online videos | Avoid deep forward bends; listen to your body |
| Pelvic tilts (cat‑cow, child’s pose) | Counters hyperlordosis, aligns pelvis | Requires no equipment | Perform slowly; stop if pain spikes |
| Acetaminophen (paracetamol) | Temporarily eases moderate pain | Generally regarded safe in pregnancy when used as directed | Never exceed recommended dose; avoid with liver issues |
Pick one or two strategies that feel comfortable and stick with them for a week. Most people notice a gentler ache within a few days.
Everyday Lifestyle Tweaks
Small habits have a surprisingly big impact:
- Footwear: Choose low‑heeled, supportive shoes. Flip‑flops and stilettos amplify forward tilt.
- Sleep position: Sleep on your side with a pillow between the knees. It keeps the pelvis neutral and eases pressure on the lumbar spine.
- Standing breaks: If your job requires you to stand, shift weight from one foot to the other every few minutes, or use a footstool.
- Carry wisely: When picking up objects, bend at the hips and knees, not at the waist. Use a small bag with a cross‑body strap instead of a heavy backpack.
When to Call Your Healthcare Provider
Most back discomfort is benign, but certain warning signs mean it’s time to get a professional opinion:
- Sudden, severe pain that doesn’t improve after rest.
- Numbness, tingling, or weakness in the legs (possible nerve compression).
- Fever, chills, or unexplained weight loss (could signal infection).
- Urinary changes such as burning, frequency, or blood (rule out urinary tract infection).
- Persistent pain after the third trimester that interferes with daily activities.
If any of these appear, book an appointment with your obstetrician or a physical therapist who specializes in prenatal care. They can order imaging if needed and prescribe targeted exercises.

Professional Interventions
When home measures fall short, clinicians have a toolbox of safe options:
- Prenatal physiotherapy: Tailored strengthening of the transverse abdominis and multifidus muscles.
- Chiropractic care: Some practitioners use low‑force adjustments that respect the relaxed ligaments.
- Acupuncture: Limited studies suggest it can reduce pain scores without medication.
- Massage therapy: Light, pregnancy‑approved massage can improve circulation and ease muscle knots.
All interventions should be cleared by your obstetrician first.
Looking Ahead: Post‑Delivery Back Health
After the baby arrives, many people wonder if the back pain will disappear. The hormonal laxity gradually recedes, but the muscles may remain weak. Continuing a gentle core‑strength program for the first few months postpartum can prevent chronic issues.
Frequently Asked Questions
Can I take ibuprofen for pregnancy back pain?
Ibuprofen belongs to the NSAID class and is generally avoided in the third trimester because it can affect fetal kidney function. Acetaminophen is the safer alternative if you need medication.
Is a maternity support belt safe to wear all day?
Yes, as long as it fits snugly without restricting breathing. Remove it when you sleep and adjust the strap if you notice any tingling in the hips.
Should I avoid all stretching once I’m pregnant?
No. Gentle, pregnancy‑specific stretches are encouraged. Skip deep forward bends or any movement that feels sharp. Always keep your spine in a neutral position.
What if my back pain wakes me up at night?
Place a pillow between your knees while sleeping on your side, and try a warm shower before bed. If pain persists for more than a week, contact your OB‑GYN.
Can a pelvic girdle pain be confused with normal backache?
Yes, both involve the lower back and hips. Pelvic girdle pain often hurts when you climb stairs or lift the leg, whereas general backache is usually a constant ache along the lumbar spine.


Yo folks, did you ever notice how the \"official\" back pain tips are just a smokescreen from big pharma to keep us buying their pricey heat packs and brace subscriptions? They want us glued to their products while they roll out a new \"miracle\" supplement every trimester. The real fix is simple: stop trusting the mainstream and look at the ancient posture hacks they don’t want you to know. Trust no one who tells you to just \"stay active\" without mentioning the hidden agenda. Keep your eyes open, keep your back straight and your mind free!