When your skin breaks out in scaly patches and your fingers or toes suddenly swell up like sausages, it’s not just coincidence. That’s the psoriatic arthritis connection in action. It’s not two separate problems - it’s one immune system gone rogue, attacking both your skin and your joints at the same time. For many people, the skin comes first. But for about 15%, the joint pain starts before any rash appears. That’s why so many get misdiagnosed for years - doctors see swollen knees or stiff fingers and think rheumatoid arthritis. But the clues are there if you know where to look.
How Skin and Joints Are Connected
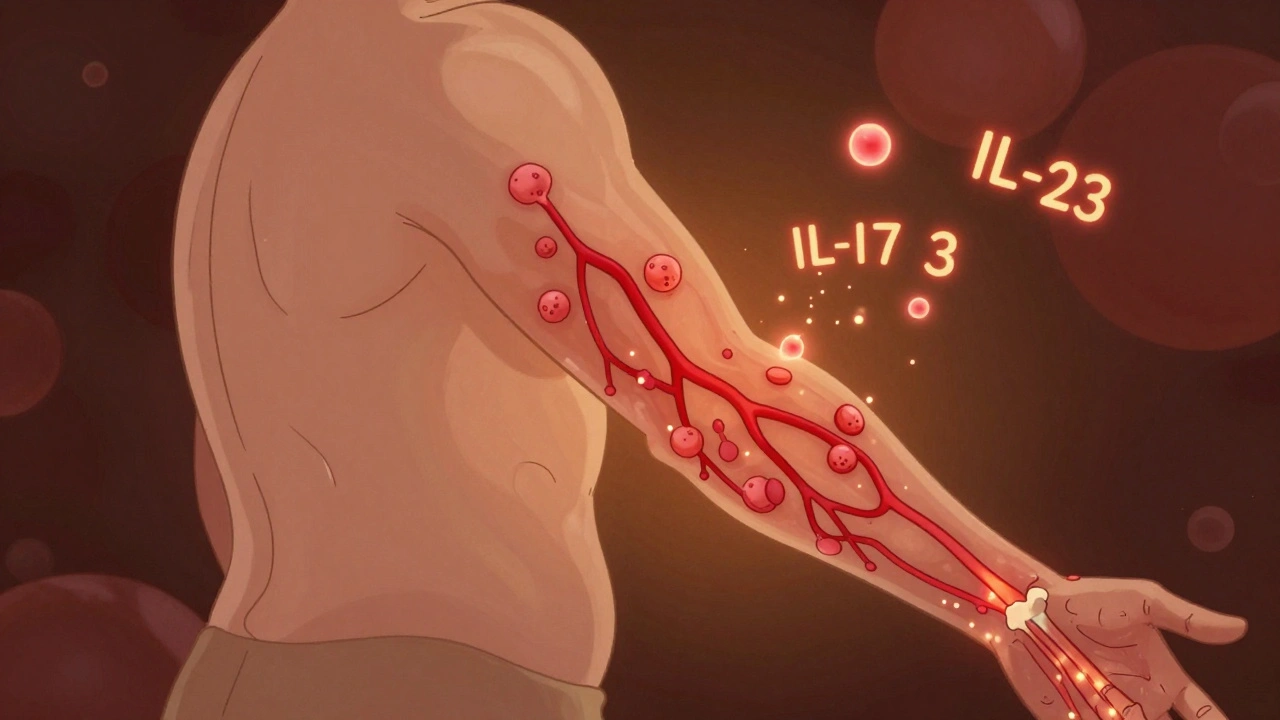
The immune system in psoriatic arthritis doesn’t just target one area. It hits the synovium - the lining of your joints - and the enthesis, where tendons and ligaments stick to bone. That’s why you get both joint pain and skin plaques. It’s the same overactive immune signal, just playing out in different places. This isn’t just about inflammation. It’s about shared biology. Studies show that the same inflammatory molecules - like IL-17 and IL-23 - drive both the red, flaky patches on your elbows and the swelling in your knuckles.
Most people with psoriatic arthritis already have plaque psoriasis - the thick, silvery scales on knees, scalp, or lower back. But even if your skin looks fine, watch your nails. Pitting, ridges, or nails lifting off the nail bed (onycholysis) are red flags. In fact, 80 to 90% of people with psoriatic arthritis have nail changes, compared to only 10 to 50% of those with psoriasis alone. That’s a major clue doctors use to spot the joint link early.
Key Signs You’re Not Just Getting Older
Joint pain from psoriatic arthritis doesn’t feel like typical wear and tear. It’s sharp, stiff, and often worse in the morning. But here’s what makes it different:
- Asymmetrical swelling: One knee hurts, the other doesn’t. Your right index finger swells, but the left one’s fine. This happens in about 70% of cases - unlike rheumatoid arthritis, which usually hits both sides evenly.
- Dactylitis: One or more fingers or toes puff up like sausages. It’s not just swelling - the whole digit looks inflamed from base to tip. Around 40 to 50% of people with psoriatic arthritis get this.
- Enthesitis: Pain where tendons meet bone. Think heel pain from plantar fasciitis or Achilles tendon pain that doesn’t go away with rest. About one in three patients have this.
- Distal joint involvement: The joints closest to your fingernails and toenails are often the first to go. If your fingertips hurt and your nails look odd, that’s a classic sign.
- Spinal stiffness: If your lower back or neck feels stiff, especially in the morning, and improves with movement, it could be spondylitis - a subtype affecting 5 to 20% of patients.
These signs don’t show up all at once. They creep in. A sore heel in January. Swollen fingers in March. A rash that flares after stress. It’s easy to brush off - until you can’t grip your coffee mug or walk without limping.
Why Diagnosis Takes So Long
There’s no blood test that confirms psoriatic arthritis. No single marker like rheumatoid factor. That’s why the average person waits over two years to get the right diagnosis. A 2022 survey found 42% of patients saw three or more doctors before being told the truth. Many are told they have osteoarthritis or tendonitis. Others get labeled with fibromyalgia because their pain doesn’t show up on X-rays - even though it’s real.
Doctors rely on a mix of signs: your skin history, joint pattern, nail changes, and imaging. Ultrasound and MRI can spot early inflammation in tendons and joints before X-rays show damage. If you have psoriasis and unexplained joint pain, insist on a rheumatology referral. Dermatologists are often the first to spot it - they see the skin changes, and about 45% of psoriatic arthritis cases are first identified by them.

Treatment: It’s Not One-Size-Fits-All
Treatment isn’t about curing - there’s no cure yet. It’s about stopping damage and keeping you moving. The goal? Minimal disease activity. That means little to no pain, no swelling, and no new joint damage.
Here’s what works:
- NSAIDs (like ibuprofen): Help with pain and swelling short-term, but don’t stop joint damage.
- DMARDs (methotrexate, sulfasalazine): Slows disease progression. Often used first if symptoms are mild.
- Biologics: These are the game-changers. They block specific parts of the immune system driving inflammation. Examples: adalimumab (Humira), etanercept (Enbrel), ustekinumab (Stelara), guselkumab (Tremfya). Many patients see 70 to 80% improvement in joint pain and skin plaques within months.
- Small molecules: Newer oral drugs like deucravacitinib (Sotyktu) target the TYK2 pathway. First approved in 2022, it’s an option for those who can’t stand injections.
Most people need combination therapy - a DMARD plus a biologic - to reach the target. But it’s not just about pills and shots. Physical therapy is critical. A 2023 study showed that patients who did regular joint mobility exercises reduced stiffness by 60% compared to those who didn’t.
Real People, Real Results
One Reddit user, ‘PsOwarrior87,’ spent five years being treated for rheumatoid arthritis. His joints kept swelling, his skin flared. When he switched to ustekinumab, his joint pain dropped 80% - but his scalp psoriasis got worse. He had to adjust his treatment plan. That’s the reality. One drug helps one part, but can trigger another.
Another user on MyHealthTeams, ‘ArthritisFree2022,’ switched to guselkumab. Morning stiffness went from two hours to 20 minutes in six weeks. She still has flare-ups, but now she knows her triggers: stress, lack of sleep, and cold weather.
But it’s not all wins. Over 78% of patients pay more than $500 a month out-of-pocket for biologics. Insurance delays average 14.7 business days. Many people skip doses because they can’t afford them. And even when joints feel better, 52% still struggle with brain fog - mental fatigue that doesn’t go away with medication.
What You Can Do Today
If you have psoriasis and notice any of these signs:
- Write down your symptoms: When did the pain start? Which joints? Did your nails change?
- Take photos of your skin and nails. Visuals help doctors spot patterns.
- Ask your dermatologist for a referral to a rheumatologist. Don’t wait for your primary care doctor to catch it.
- Start tracking triggers: Stress, alcohol, infections, weather. Many patients notice flare-ups after strep throat or during winter.
- Ask about screening: Before starting biologics, you’ll need tests for TB and hepatitis. Do them early - delays can cost you months.
Early treatment within 12 weeks of symptoms starts can prevent 75% of irreversible joint damage, according to rheumatologists at Oxford. Waiting just six months can mean the difference between managing pain and needing joint replacements.
The Future Is Getting Better
AI is now predicting who will develop psoriatic arthritis from their psoriasis - with 87% accuracy - using nail images and joint scans. Clinical trials for new oral JAK inhibitors are wrapping up in late 2024. By 2028, genetic testing may match patients to the best drug before they even start treatment, cutting out the trial-and-error phase.
But for now, the most powerful tool you have is awareness. If your skin and joints are both acting up, don’t ignore it. Don’t assume it’s aging. Don’t settle for painkillers that only mask the problem. The link between your skin and your joints is real - and treating it early changes everything.
Can psoriatic arthritis happen without skin psoriasis?
Yes, but it’s rare. About 15% of people develop joint symptoms before any visible skin rash appears. These cases are harder to diagnose because doctors don’t immediately connect the joint pain to psoriasis. If you have a family history of psoriasis and suddenly get unexplained joint swelling or stiffness, tell your doctor - even if your skin looks fine.
Is psoriatic arthritis the same as rheumatoid arthritis?
No. Rheumatoid arthritis usually affects joints symmetrically - both hands, both knees. Psoriatic arthritis often hits joints on just one side. It also causes dactylitis (sausage fingers), enthesitis (tendon pain), and nail changes, which are rare in rheumatoid arthritis. Blood tests also differ: rheumatoid factor is positive in most rheumatoid cases, but negative in 90% of psoriatic arthritis cases.
Do biologics cure psoriatic arthritis?
No, they don’t cure it. But they can put the disease into long-term remission. Many patients achieve minimal disease activity - meaning little to no pain, swelling, or joint damage. Stopping biologics often leads to flare-ups, so most people stay on them long-term. The goal is control, not cure.
Can diet or supplements help with psoriatic arthritis?
No supplement or diet has been proven to stop joint damage. But some people report less inflammation with omega-3s, vitamin D, or avoiding alcohol and processed sugar. These aren’t replacements for medication, but they can support overall health. Always talk to your doctor before starting anything new - some supplements can interfere with biologics.
How do I know if my treatment is working?
Track your symptoms: How long is your morning stiffness? Can you grip objects? Are your nails improving? Your doctor will use tools like the Psoriatic Arthritis Disease Activity Score (PASDAS) or check for minimal disease activity - defined as fewer than 3 tender joints, fewer than 2 swollen joints, no enthesitis, and low skin involvement. If you’re not improving after 3 to 6 months, ask about switching therapies.


man i thought i was just getting old till my knuckles swelled up like little sausages and my scalp started flaking like a christmas tree
turns out my body was just throwing a tantrum
psoriatic arthritis is wild like that