Renal Dosing Calculator for Metformin and SGLT2 Inhibitors
Enter your eGFR value to determine appropriate dosing for metformin and SGLT2 inhibitors based on the latest clinical guidelines.
When you have type 2 diabetes and chronic kidney disease, choosing the right medication isn’t just about lowering blood sugar-it’s about protecting your kidneys, avoiding harm, and staying alive longer. Two of the most important drugs for this job are metformin and SGLT2 inhibitors. But their dosing changes based on how well your kidneys are working. Get it wrong, and you risk lactic acidosis, dehydration, or missing out on life-saving kidney protection. Get it right, and you can slow kidney decline by up to 40%.
Why Kidney Function Changes Everything
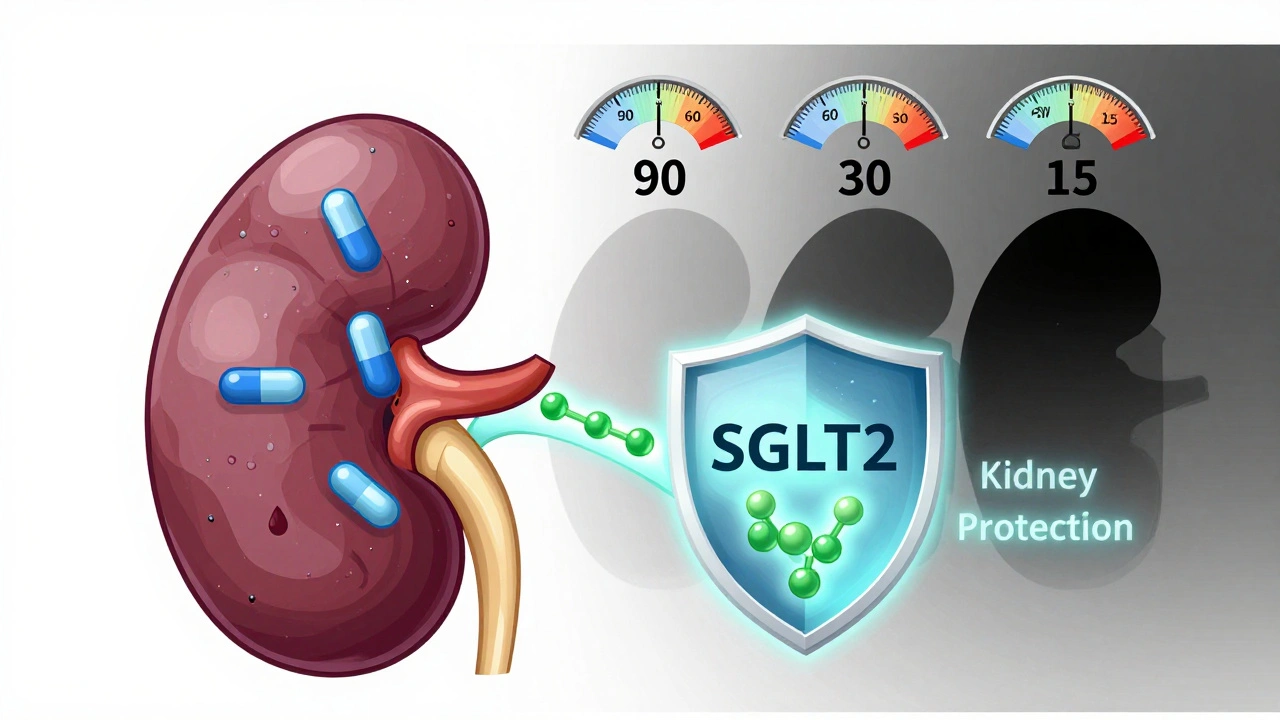
Your kidneys don’t just filter waste-they help clear drugs from your body. When kidney function drops, these medications build up. That’s dangerous with metformin, which can cause lactic acidosis if too much stays in your blood. With SGLT2 inhibitors, low kidney function means less sugar gets pulled into your urine, so the drug seems to stop working. But here’s the twist: even when they seem less effective, they’re still protecting your kidneys.The key number doctors look at is your eGFR-estimated glomerular filtration rate. It’s a blood test that tells you how well your kidneys filter. Normal is 90 or above. Below 60 means chronic kidney disease. And your treatment plan changes at every major drop.
Metformin: The Old Rules Are Gone
Ten years ago, if your eGFR fell below 60, you were told to stop metformin. That’s not true anymore. In 2016, the FDA updated its safety warning after studies showed the risk of lactic acidosis was extremely low-just 3.3 cases per 100,000 patient-years. That’s less than being struck by lightning.Today, the guidelines are clear:
- eGFR ≥60 mL/min/1.73 m²: Max dose is 2550 mg per day
- eGFR 45-59 mL/min/1.73 m²: Max dose is 2000 mg per day
- eGFR 30-44 mL/min/1.73 m²: Max dose is 1000 mg per day
- eGFR <30 mL/min/1.73 m²: Do not start metformin. If already on it, stop.
Some doctors will still give 500 mg daily to patients with eGFR between 15 and 30 if they’re stable and closely monitored. But that’s off-label and not recommended by most guidelines. The goal? Keep using metformin as long as safely possible. It cuts heart attacks, strokes, and death by up to 30% in people with diabetes and kidney disease.
SGLT2 Inhibitors: The Kidney Protectors
SGLT2 inhibitors-like dapagliflozin, empagliflozin, and canagliflozin-were originally designed to lower blood sugar. But the real breakthrough came when trials showed they reduced kidney failure, heart attacks, and death in people with diabetes and kidney disease. The DAPA-CKD trial (2020), EMPA-KIDNEY (2022), and CREDENCE (2019) proved this beyond doubt.Before 2022, most guidelines said you could only use SGLT2 inhibitors if your eGFR was 30 or higher. Now? The Kidney Disease: Improving Global Outcomes (KDIGO) guidelines say you can start them at eGFR ≥20 mL/min/1.73 m². That’s a big deal. It means more people get the benefit.
But each drug has its own rules:
- Canagliflozin: Max 100 mg/day if eGFR 45-59; stop if eGFR <45
- Dapagliflozin: Max 10 mg/day if eGFR 25-45; stop if eGFR <25
- Empagliflozin: Max 10 mg/day if eGFR 30-45; stop if eGFR <30
Here’s the catch: KDIGO says you can keep using SGLT2 inhibitors even if your eGFR drops below 20-as long as you’re not on dialysis and you’re not having side effects. That’s different from the FDA’s labeling. The FDA still says canagliflozin is contraindicated below eGFR 45. That’s why some doctors stop the drug even when it’s working.
The Narrow Window: eGFR 20-29
This is the trickiest zone. Your eGFR is too low for metformin (which needs ≥30), but high enough for SGLT2 inhibitors (which work down to 20). So what do you do?Stop metformin. Start or continue an SGLT2 inhibitor. That’s the recommendation from KDIGO and the American Diabetes Association. In this range, you’re losing kidney protection if you don’t use an SGLT2 inhibitor. But you’re risking lactic acidosis if you keep metformin.
One patient I saw had an eGFR of 24. She was on metformin 1000 mg daily. We stopped it. Started dapagliflozin 10 mg. Three months later, her albuminuria dropped by 50%. Her eGFR dipped to 21-expected. We didn’t stop the drug. Her blood pressure stayed stable. Her sugar improved. She’s still on it two years later.
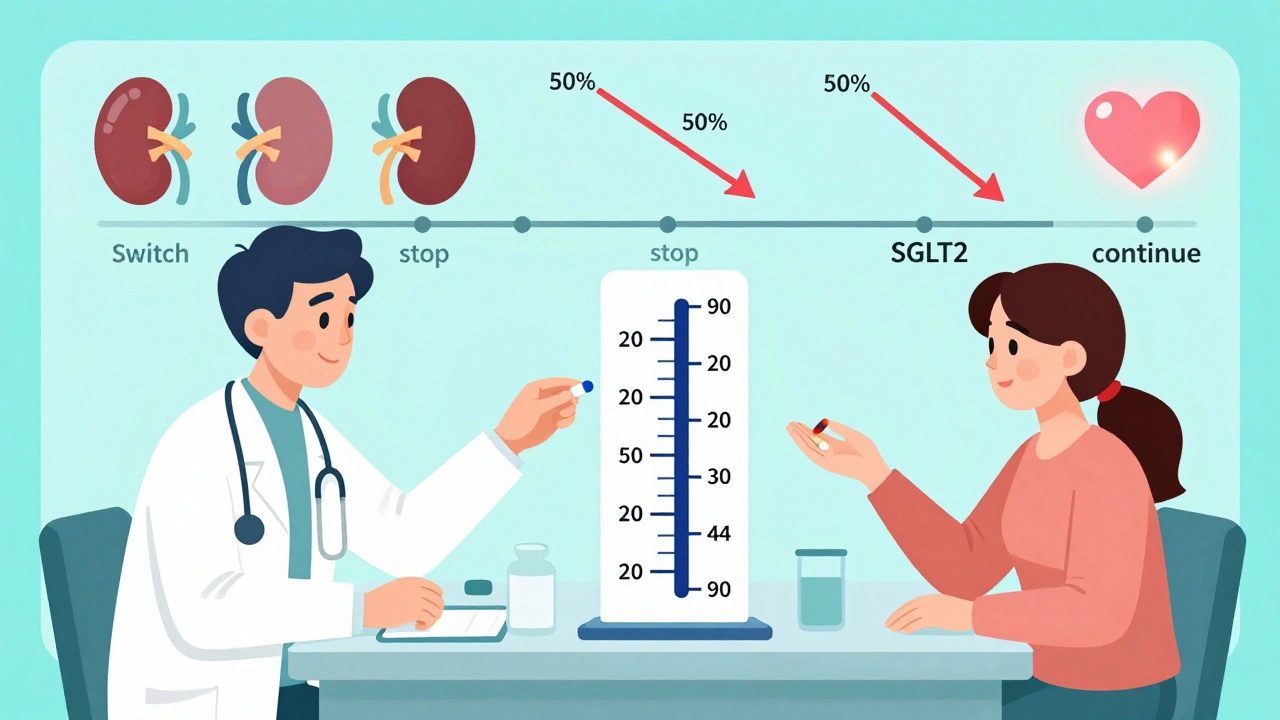
What About That eGFR Drop?
When you start an SGLT2 inhibitor, your eGFR often drops by 2-5 mL/min/1.73 m² in the first few weeks. That’s not kidney damage. That’s the drug doing its job. It reduces pressure inside the kidney’s filtering units, which protects them long-term.But many doctors panic. They see the drop, think the drug is hurting the kidneys, and stop it. That’s a mistake. The UK Kidney Association says clearly: “A decline in eGFR needs to be interpreted with caution and in the context of an expected drug effect.”
Track it. Wait 3-6 months. If it stabilizes or improves, keep going. If it keeps falling fast, look for other causes-dehydration, heart failure, infection, or another medication.
Monitoring: How Often to Check
You can’t set it and forget it. Here’s the monitoring schedule that works:- Metformin users:
- eGFR ≥60: Check every 6-12 months
- eGFR 45-59: Check every 3-6 months
- eGFR 30-44: Check every 3 months
- SGLT2 inhibitor users:
- Check eGFR before starting
- Check again at 4-6 weeks
- Then every 3-6 months if stable
Also check for signs of dehydration-dizziness, low blood pressure, dry mouth. SGLT2 inhibitors make you pee more. If you’re also on a diuretic (like furosemide), you’re at higher risk for low blood pressure or acute kidney injury. Tell your doctor if you’re sick, vomiting, or not drinking enough.
What Happens on Dialysis?
There’s no perfect data here, but here’s what we know:- Metformin: Avoid. Even on dialysis, it builds up. Some sources say 250 mg after peritoneal dialysis, or 500 mg after hemodialysis-but this is risky and not standard.
- SGLT2 inhibitors: Not effective. They work by pulling sugar into the urine. No urine? No benefit. Stop them.
If you’re on dialysis, your diabetes management shifts to insulin or other non-kidney-dependent drugs. SGLT2 inhibitors and metformin are out.
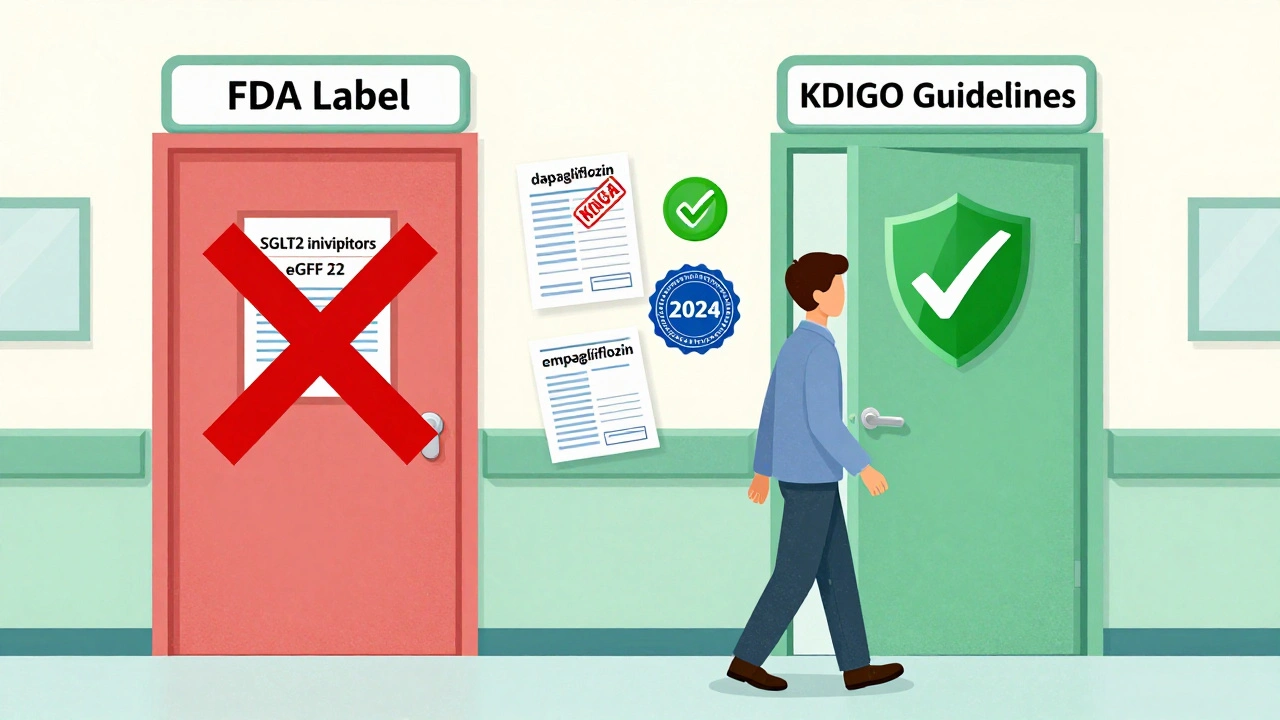
Insurance and the Real-World Mess
Here’s the ugly truth: guidelines say one thing. Insurance says another.A 2022 survey found that 43% of endocrinologists had claims denied for SGLT2 inhibitors when eGFR was between 20 and 29-even though KDIGO says it’s safe and effective. Insurance companies still follow FDA labels, not clinical guidelines. So your doctor might have to appeal, write letters, or switch you to a drug with a higher eGFR threshold.
And then there’s the gap between primary care and nephrology. One doctor sees the FDA label and stops the drug. The nephrologist says, “Keep it. It’s protecting her kidneys.” That conflict causes delays, frustration, and sometimes harm.
The Future: What’s Coming
In February 2024, the FDA approved dapagliflozin for chronic kidney disease-even if you don’t have diabetes. That’s huge. It means SGLT2 inhibitors are now recognized as kidney protectors, not just diabetes drugs.By 2025, we’ll likely see updated guidelines that include use in eGFR 15-19. Some experts are already studying whether these drugs help people with eGFR below 15. Early data is promising.
Right now, the message is clear: don’t stop SGLT2 inhibitors because of a small eGFR dip. Don’t withhold metformin when it’s still safe. And don’t let insurance rules override science. Your kidneys need these drugs more than ever.
What to Do Now
If you have diabetes and kidney disease:- Ask your doctor for your latest eGFR number.
- Ask: “Am I on the right dose of metformin based on my kidney function?”
- Ask: “Should I be on an SGLT2 inhibitor? If not, why not?”
- Ask: “What should I do if my eGFR drops?”
- Keep your kidney tests on schedule. Don’t skip them.
This isn’t about taking more pills. It’s about staying alive longer, avoiding dialysis, and keeping your heart strong. The science is clear. The tools are here. Now it’s about using them right.
Can I still take metformin if my eGFR is 35?
Yes, but you must reduce your dose to no more than 1000 mg per day. This is the maximum safe dose for eGFR between 30 and 44 mL/min/1.73 m². Your doctor should monitor your kidney function every 3 months. Do not increase the dose unless your eGFR improves.
Why did my doctor stop my SGLT2 inhibitor when my eGFR dropped to 22?
Your doctor may have followed FDA labeling, which still lists higher eGFR thresholds for some SGLT2 inhibitors (like canagliflozin, which is contraindicated below 45). But according to the 2022 KDIGO guidelines, you can safely continue SGLT2 inhibitors down to eGFR 20 and even below if you tolerate them. Ask for a second opinion from a nephrologist if your kidney function is stable and you’re not having side effects.
Is it safe to take metformin and an SGLT2 inhibitor together?
Yes, and it’s often the best combination for people with diabetes and early to moderate kidney disease. The ADA and KDIGO recommend starting both together if your eGFR is ≥30. Metformin controls blood sugar and reduces heart risks. SGLT2 inhibitors protect your kidneys and heart. Together, they cut the risk of kidney failure by 30-40%. Just avoid the combo if your eGFR is below 30.
What should I do if I get sick and can’t eat or drink?
Stop both metformin and SGLT2 inhibitors temporarily. Illness, vomiting, diarrhea, or dehydration can cause your eGFR to drop suddenly and increase your risk of lactic acidosis or acute kidney injury. Call your doctor. Restart only after you’re eating, drinking, and your kidneys are back to normal.
Can SGLT2 inhibitors help if I don’t have diabetes?
Yes. In February 2024, the FDA approved dapagliflozin for chronic kidney disease even if you don’t have diabetes. It works by reducing pressure and inflammation in the kidneys. If you have albuminuria (protein in urine) and an eGFR above 25, this drug can slow kidney decline. Guidelines are moving toward using SGLT2 inhibitors for all patients with CKD and proteinuria, regardless of diabetes status.


Metformin at eGFR 35? Just keep it at 1000mg and move on. No need to overthink it.