When you’re pregnant or breastfeeding, every pill, supplement, or remedy feels like a gamble. You want relief from migraine pain - but not at the cost of your baby’s health. The truth? You don’t have to choose between suffering and safety. Many effective, low-risk options exist if you know what to look for.
Why Migraines Change During Pregnancy
For about 60 to 70% of women, migraines improve during pregnancy, especially in the second and third trimesters. That’s thanks to rising estrogen levels, which stabilize brain activity linked to migraine triggers. But for others, migraines get worse - especially right after delivery, when estrogen drops sharply. This isn’t just about headaches. Untreated migraines raise your risk of preterm birth, preeclampsia, and low birth weight. A 2020 study of over 114,000 pregnancies found that women with frequent migraines had a 14.3% chance of preeclampsia, compared to 6.2% in those without migraines.First-Line Defense: Non-Drug Treatments
Before reaching for medication, try these proven, zero-risk strategies. They’re not just "natural" - they’re backed by science.- Sleep 7-9 hours a night. Poor sleep is one of the top migraine triggers. Keep a consistent schedule, even on weekends.
- Move daily. Thirty minutes of walking, swimming, or prenatal yoga five days a week reduces migraine frequency by up to 40%.
- Stay hydrated. Drink 2-3 liters of water daily. Dehydration triggers migraines in up to 30% of pregnant women.
- Try acupuncture. A 2021 trial with 120 pregnant women showed 68% had at least a 50% drop in migraine days after 8 weeks of weekly sessions.
- Use massage therapy. Two 30-minute sessions per week in the second and third trimesters cut migraine frequency by 35%.
- Try Cefaly. This FDA-cleared headband stimulates the trigeminal nerve. In studies, 68% of users saw migraine frequency drop by half - and it’s safe during pregnancy and breastfeeding.
Safe Pain Relief During Pregnancy
If non-drug methods aren’t enough, acetaminophen (Tylenol) is your best bet. It’s the only over-the-counter painkiller recommended throughout pregnancy. Take up to 3,000 mg per day - no more. Studies tracking over 1,200 pregnancies found no link to birth defects. Sumatriptan (Imitrex) is also considered safe for acute attacks. Three large studies and two systematic reviews show no increase in major birth defects above the normal 3% rate. But here’s the catch: using triptans in the second or third trimester may slightly raise the risk of heavy bleeding after delivery and uterine atony. So use them only when necessary, and only after discussing with your doctor. Avoid these completely:- Ergots (like Cafergot): Can trigger dangerous uterine contractions.
- Valproic acid: Increases neural tube defect risk by 11%.
- Feverfew: Linked to a 38% higher chance of miscarriage.
Migraine Prevention During Pregnancy
If you get migraines more than twice a week, prevention matters. Magnesium is the top choice. Take 400-600 mg daily. A 2021 Cochrane review of 550 pregnant women found it cut migraine frequency by 35% with no side effects to mom or baby. Propranolol (a beta-blocker) can help prevent migraines, but it’s not first-line. Studies show a 15% higher risk of slow fetal growth and small placenta. Use it only if other options fail and under close monitoring. Cyclobenzaprine (a muscle relaxant) has been used in 127 pregnancies with no major malformations reported. Memantine is theoretically low-risk due to high protein binding, but data is limited. Talk to your neurologist before starting anything.
Safe Options While Breastfeeding
Breastfeeding opens up more options. The key is the Relative Infant Dose (RID) - how much of the drug ends up in breast milk. Anything under 10% is considered safe.- Acetaminophen: RID 8.81% - safe, no restrictions.
- Ibuprofen: RID 0.65% - even safer than acetaminophen, and works well for inflammation.
- Sumatriptan: RID 3.0% - classified as L1 (safest). Take it right after nursing, then wait 3-4 hours before the next feed to let levels drop.
- Rizatriptan: RID 1.2% - limited data, but looks promising.
- Metoclopramide: RID 0.5% - helps with nausea and can ease migraine symptoms.
- Ondansetron: RID 0.7% - safe for nausea and vomiting linked to migraines.
- Verapamil: RID 0.15-0.2% - lowest among calcium channel blockers. Safe and effective.
- Propranolol: RID 0.3-0.5% - fine, but watch your baby for drowsiness or slow heart rate.
- Amitriptyline: RID 1.9-2.8% - one of the safest antidepressants for migraine prevention while nursing.
- Sertraline: RID 0.4-2.2% - also safe, with added benefit for postpartum mood.
- Magnesium sulfate and riboflavin (B2): Both L1 classified. Riboflavin isn’t well studied for migraine prevention in nursing moms, but it’s safe to try at 400 mg/day.
What About Newer Drugs Like Nurtec?
Rimegepant (Nurtec ODT), approved by the FDA in 2023, is now an option for both acute and preventive treatment. It’s classified as L2 for breastfeeding - meaning it’s likely safe, but data is still limited. No pregnancy data exists yet, so avoid it during gestation unless absolutely necessary and under specialist care. CGRP inhibitors (like Aimovig, Emgality) are great for chronic migraine - but their safety in pregnancy hasn’t been studied enough. Hold off until more evidence is available.Timing Matters: How to Take Meds Safely While Nursing
Even safe drugs can build up if taken at the wrong time. The golden rule: take your medication right after you finish nursing. That gives your body 3-4 hours to clear most of the drug before the next feeding. For example: Nurse at 8 PM, take your sumatriptan at 8:30 PM. Next feed is 12 AM - you’ve got 3.5 hours of clearance. Most babies sleep longer at night, making this timing easier.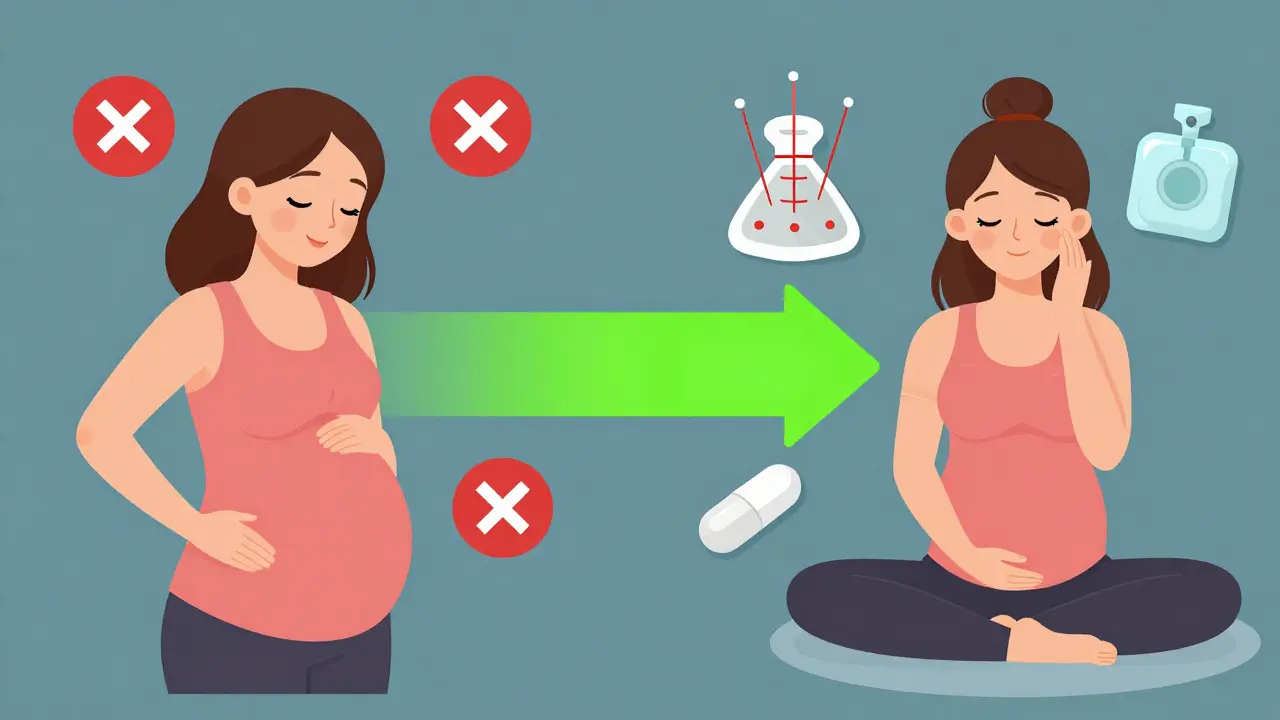
Real Stories, Real Results
A 2023 survey of 1,247 breastfeeding mothers found 78% managed migraines with just acetaminophen and ibuprofen - no interruptions to breastfeeding. Only 15% needed triptans, and 92% reported no changes in their babies’ behavior or feeding. On Reddit’s r/Migraine forum, over 60% of 347 posts mentioned success with non-drug tools: yoga, Cefaly, ice packs, and strict sleep routines. One mom wrote: "I used to have 10 migraines a month. After starting magnesium and Cefaly, I had two in six months. I’m nursing my second baby and haven’t taken a pill since week two."What Your Doctor Might Not Tell You
A 2022 survey found that 42% of obstetricians and 68% of neurologists feel undertrained in managing migraines during pregnancy. That means you might need to lead the conversation. Bring this info to your appointments. Ask: "What’s the RID of this drug?" or "Is there a non-drug option I can try first?" If your provider doesn’t know, ask for a referral to a headache specialist or lactation consultant certified by IBLCE.When to Worry
Migraine isn’t just a headache. If you develop:- Sudden, "thunderclap" pain
- Vision loss, confusion, or weakness on one side
- High blood pressure or swelling in hands/face
Bottom Line: You Can Live Well
You don’t have to suffer through pregnancy or breastfeeding with unmanaged migraines. The safest path is simple: start with sleep, hydration, movement, and magnesium. Add non-drug tools like Cefaly or acupuncture. Use acetaminophen or ibuprofen for breakthrough pain. If you need a triptan, take it right after nursing. Avoid ergots, valproate, and feverfew entirely. Untreated migraines hurt more than treated ones. High stress, sleep loss, and depression from constant pain can affect your baby’s development more than properly chosen medications. You’re not being reckless by treating your pain - you’re being responsible.Is it safe to take Tylenol while pregnant for migraines?
Yes, acetaminophen (Tylenol) is the safest pain reliever during pregnancy. Studies tracking over 1,200 pregnancies found no increased risk of birth defects when taken at doses up to 3,000 mg per day. It’s the first-line recommendation from the American College of Obstetricians and Gynecologists.
Can I take sumatriptan while breastfeeding?
Yes, sumatriptan is considered safe during breastfeeding. It has a low Relative Infant Dose (RID) of 3.0%, classified as L1 (safest) by Hale’s criteria. To minimize exposure, take it right after nursing and wait 3-4 hours before the next feed. Most babies show no side effects.
What migraine medications should I avoid during pregnancy?
Avoid ergots (like Cafergot), valproic acid, and feverfew. Ergots can cause dangerous uterine contractions. Valproic acid increases the risk of neural tube defects by 11%. Feverfew is linked to a 38% higher chance of miscarriage. These are not safe at any stage of pregnancy.
Does magnesium help prevent migraines during pregnancy?
Yes. A 2021 Cochrane Review of 8 trials with 550 pregnant women found that taking 400-600 mg of magnesium daily reduced migraine frequency by 35%. It has no known risks to the baby and is recommended as a first-line preventive option.
Is Cefaly safe to use while pregnant and breastfeeding?
Yes. Cefaly is a non-drug, FDA-cleared device that stimulates the trigeminal nerve. Studies show a 50% reduction in migraine frequency in 68% of users. It has no systemic absorption, so it’s completely safe during pregnancy and breastfeeding. No medications or side effects involved.
What should I do if my migraines get worse after giving birth?
Postpartum migraine spikes are common due to plummeting estrogen. Start with non-drug strategies: sleep when the baby sleeps, stay hydrated, use ice packs, and try Cefaly. If you need medication, acetaminophen and ibuprofen are safe. If migraines are severe or frequent, talk to your doctor about low-risk preventive options like magnesium, verapamil, or sertraline.



OMG YES!!! This is the guide I wish I had when I was pregnant!! I thought I was doomed to 10 migraines a month until I tried Cefaly and magnesium-and now my toddler doesn’t even remember me being in bed with ice packs!! 🙌🙌🙌