Hyponatremia Risk Calculator
Medication Risk Assessment
This tool helps you understand your risk of severe hyponatremia caused by medications. Based on the article's research, 61% of severe cases occur in patients over 65, and 57% in women.
When your sodium levels drop too low, your brain starts to swell. It’s not a slow, quiet process-it can happen in hours. And the most common cause? Medications you’re taking for depression, high blood pressure, or seizures. This isn’t rare. Every year, thousands of people end up in the hospital because their body can’t handle the way a drug is messing with their electrolytes. The symptoms start small: a headache, feeling off, maybe nausea. But if you ignore them, you could end up having a seizure, slipping into confusion, or worse. This is serious. And it’s preventable-if you know what to look for.
What Exactly Is Hyponatremia?
Hyponatremia means your blood sodium is below 135 mmol/L. Severe hyponatremia kicks in when it drops below 120 mmol/L. Sodium isn’t just about salt on your food. It’s the key electrolyte that keeps your cells balanced, especially in your brain. When sodium drops too fast, water rushes into brain cells to balance things out. Your brain doesn’t have room to expand. It swells. And that’s when things go wrong.
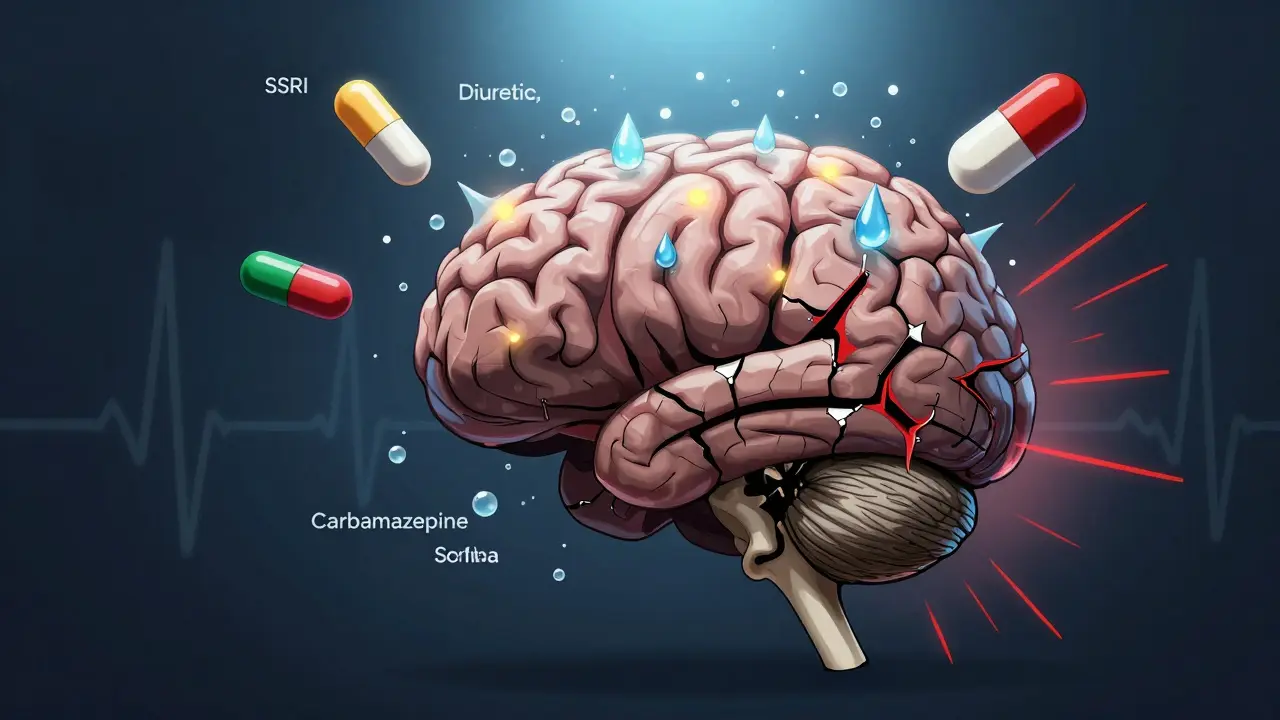
Medications are responsible for nearly one in five cases of severe hyponatremia in hospitals. The biggest culprits? Diuretics (water pills), SSRIs like sertraline and citalopram, and antiseizure drugs like carbamazepine and oxcarbazepine. Even common painkillers like ibuprofen can trigger it in vulnerable people. The problem isn’t the drug itself-it’s how your body reacts to it, especially if you’re older, female, or taking more than one medication.
The Warning Signs: Confusion, Seizures, and More
Early symptoms are easy to miss. You might think you’ve got the flu, or you’re just stressed. But if you’ve started a new medication in the last few weeks, pay attention.
- Confusion or disorientation - This is the most common sign. People forget names, get lost in familiar places, or can’t follow simple conversations. In 68% of severe cases, this is the first red flag.
- Headaches and nausea - Often dismissed as side effects. But if they come with dizziness or fatigue, they’re not just "normal."
- Seizures - When sodium drops below 115 mmol/L, about 1 in 5 people will have a seizure. It’s not epilepsy. It’s your brain drowning in water.
- Loss of balance, muscle weakness, or cramps - Your nerves can’t fire right without enough sodium.
- Coma or death - If untreated, severe hyponatremia kills. Studies show a 37% death rate if sodium stays below 115 mmol/L for more than 48 hours.
One nurse on Reddit shared a case: a 72-year-old man started sertraline for depression. Within 10 days, his sodium dropped from 138 to 118. He had a grand mal seizure. His doctor had called his headaches and nausea "typical side effects." By the time they tested his sodium, it was too late.
Why Do Medications Cause This?
Most drug-induced hyponatremia happens because of something called SIADH-Syndrome of Inappropriate Antidiuretic Hormone Secretion. Normally, your body releases ADH when you’re dehydrated to hold onto water. But some drugs trick your body into making too much ADH, even when you’re not dehydrated. Your kidneys keep reabsorbing water, diluting your blood. Sodium gets washed out.
SSRIs are the worst offenders here. They increase serotonin, which directly stimulates ADH release. Carbamazepine does the same. Even some blood pressure meds like ACE inhibitors can mess with kidney function enough to lower sodium. And it doesn’t take long. Most cases show up within 1 to 4 weeks after starting the drug. The first 30 days are the most dangerous.
Here’s who’s at highest risk:
- People over 65 - 61% of severe cases
- Women - 57% of cases
- Those taking multiple high-risk drugs
- People with low body weight or existing kidney issues
How Doctors Miss It (And How You Can Help)
Here’s the scary part: 15 to 20% of medication-induced hyponatremia cases are misdiagnosed. Patients are sent to psychiatrists for "anxiety" or "early dementia." Others are told they have the flu. Why? Because the symptoms look like other conditions. And most doctors don’t check sodium unless someone’s obviously sick.
But there’s a pattern. If you’ve started a new medication and then started feeling weird, that’s not a coincidence. A 2023 study found that 73% of severe cases develop within the first 30 days of starting a high-risk drug. Yet, only 63% of doctors follow the recommended monitoring guidelines.
What you can do:
- Ask your doctor: "Could this drug affect my sodium?" before starting it.
- Request a blood test for sodium 7 to 10 days after starting the medication, especially if you’re over 65.
- Keep a symptom journal: headaches, nausea, confusion, fatigue. Note when they started.
- If you’re on an SSRI or antiseizure drug and feel off, don’t wait. Get your sodium checked.
One Mayo Clinic patient shared how their pharmacist caught a dangerous interaction before they even filled a prescription for oxcarbazepine. "My sister had seizures from this drug," they wrote. "The pharmacist asked if I’d had any headaches. I said yes. He called my doctor. I never took it."
Treatment: Fast, But Careful
If your sodium is dangerously low, you need treatment-fast. But here’s the catch: correcting it too quickly can kill you too.
When sodium drops slowly over days, your brain adapts. But when it crashes fast-like from a new drug-the brain doesn’t have time to adjust. Fixing it too fast can cause a rare but devastating condition called osmotic demyelination syndrome, where the brain’s protective coating gets destroyed. That can leave you paralyzed, unable to speak, or in a locked-in state.
So treatment has to be precise:
- Stop the offending drug immediately.
- Restrict fluids-no extra water, no sports drinks.
- Correct sodium slowly: no more than 4 to 8 mmol/L per day.
- In severe cases, doctors may use hypertonic saline or newer drugs like tolvaptan (Samsca), approved in late 2023 for this exact use.
Recovery rates are good if caught early: 92% recover fully if treated within 24 hours. But if you wait 48 hours or longer, that drops to 67%. And for every hour you delay, your risk of permanent brain damage rises.

What Comes Next: Prevention and New Tools
It’s not enough to just treat it. We need to stop it before it starts.
Some hospitals are now using AI to predict hyponatremia risk. Mayo Clinic’s pilot system analyzes your EHR-medications, age, lab history-and flags high-risk patients 72 hours before symptoms appear. Accuracy? 87%. That’s huge.
In Europe, pharmacists now have to give sodium monitoring instructions when dispensing high-risk drugs. The FDA now requires stronger warnings on 27 medications. But in community clinics? Only 47% follow the guidelines.
Here’s the bottom line: if you’re on an SSRI, diuretic, or antiseizure drug, don’t assume you’re fine. Ask for a sodium test after 7 days. If you feel confused, dizzy, or have a headache you can’t explain, get checked. Don’t wait for a seizure. The window between feeling off and losing control can be as short as 6 to 8 hours.
Medications save lives. But they can also sneak up on you. The difference between a full recovery and permanent damage often comes down to one question: "Did anyone check my sodium?"
What to Do If You Suspect Hyponatremia
If you or someone you know is on a high-risk medication and shows signs of confusion, nausea, or weakness:
- Stop drinking extra water. This makes it worse.
- Call your doctor immediately. Say: "I’m on [medication] and I think I might have low sodium."
- If symptoms are severe-seizures, coma, extreme confusion-go to the ER. Don’t wait.
- Bring a list of all medications, including over-the-counter drugs and supplements.
- Ask for a serum sodium test. Don’t accept a vague answer.
There’s no substitute for action. If you’re worried, get tested. It takes 5 minutes. The cost? A simple blood draw. The risk of not doing it? Brain damage or death.
Can antidepressants really cause seizures from low sodium?
Yes. SSRIs like sertraline, citalopram, and fluoxetine are among the top causes of medication-induced hyponatremia. They trigger SIADH, which causes your body to hold onto too much water and dilute sodium. When sodium drops below 115 mmol/L, seizures can occur. Studies show 22% of patients with sodium levels this low have seizures. This isn’t rare-it’s a known side effect, and many doctors don’t monitor for it.
How long does it take for hyponatremia to develop from a new medication?
Most cases appear within 1 to 4 weeks after starting the drug. But 73% of severe cases happen within the first 30 days. The fastest drops can occur in under 10 days, especially in older adults. That’s why guidelines recommend checking sodium levels 7 to 10 days after starting high-risk drugs like SSRIs or carbamazepine.
Is hyponatremia from medication permanent?
No-if caught early, it’s fully reversible. Most people recover completely if sodium is corrected slowly and the drug is stopped. But if correction is too fast, it can cause osmotic demyelination syndrome, which leads to permanent brain damage. And if sodium stays too low for more than 48 hours, the risk of death or permanent disability increases dramatically.
Can I still take my medication if I’ve had hyponatremia before?
It depends. If the drug is essential-like an SSRI for severe depression-you may need to continue it. But you’ll need strict monitoring: sodium checks every 3-5 days for the first month, then monthly. For some drugs like diuretics, alternatives exist. For others, like carbamazepine, the risk is so high that switching medications is often the safest choice. Never restart the drug without medical supervision.
Why don’t doctors test sodium more often?
Many doctors don’t think about it. Hyponatremia symptoms mimic anxiety, depression, or aging. There’s no routine screening requirement in most clinics. Only 63% of prescribers follow FDA-recommended monitoring. But studies show that when sodium checks are built into protocols, misdiagnosis drops from 31% to under 5%. It’s not that doctors are careless-it’s that the system doesn’t make it easy to spot.


i started sertraline last month and got this weird headache that wouldn’t go away… thought it was just stress. now i’m scared to even look at my pill bottle. should i get blood work or just wait it out??