Statin Myopathy Risk Calculator
Statin Myopathy Risk Assessment
This tool helps you understand your personal risk for statin-induced muscle pain and myopathy based on your health characteristics. Remember: this is a general assessment, not a substitute for professional medical advice.
More than 39 million Americans take statins every year. They’re one of the most prescribed drugs in history, proven to slash heart attacks and strokes by lowering LDL cholesterol. But for a significant number of people, the benefit comes with a painful cost: muscle pain, weakness, and cramps that don’t go away. This isn’t just a minor inconvenience. It’s called statin-induced myopathy, and it’s the reason nearly one in three people stop taking their statins.
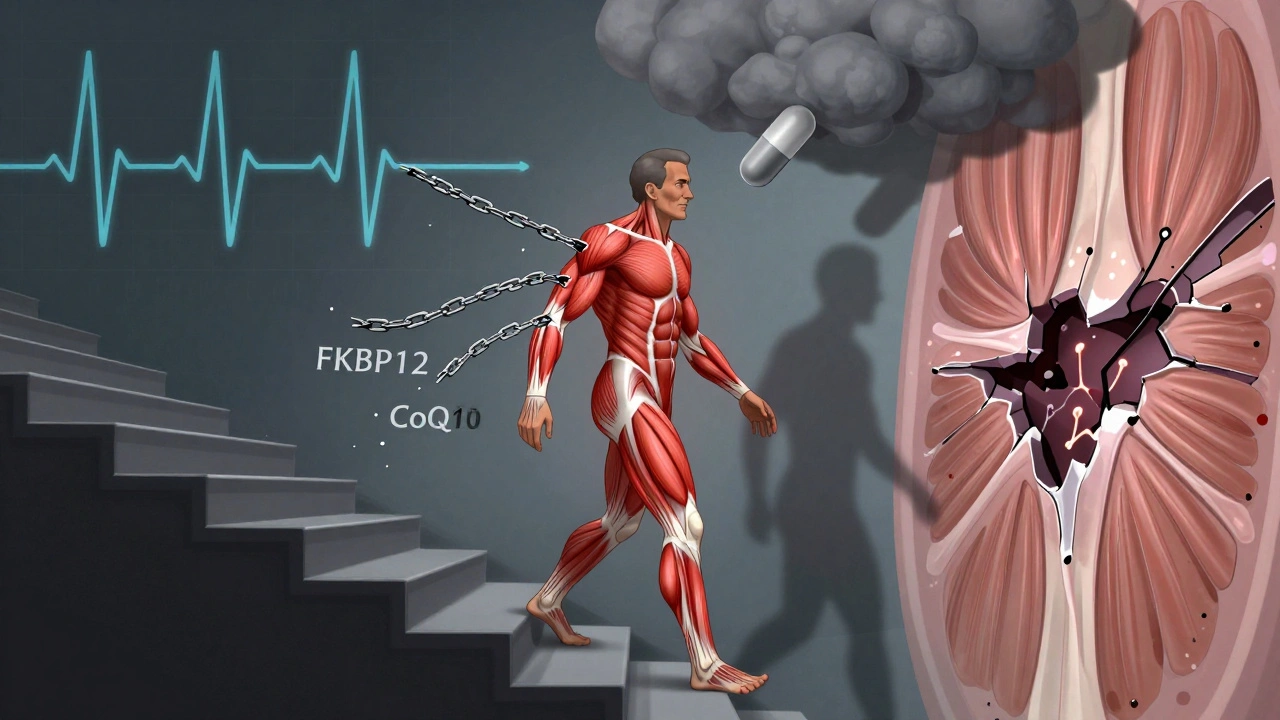
How Statins Trigger Muscle Damage
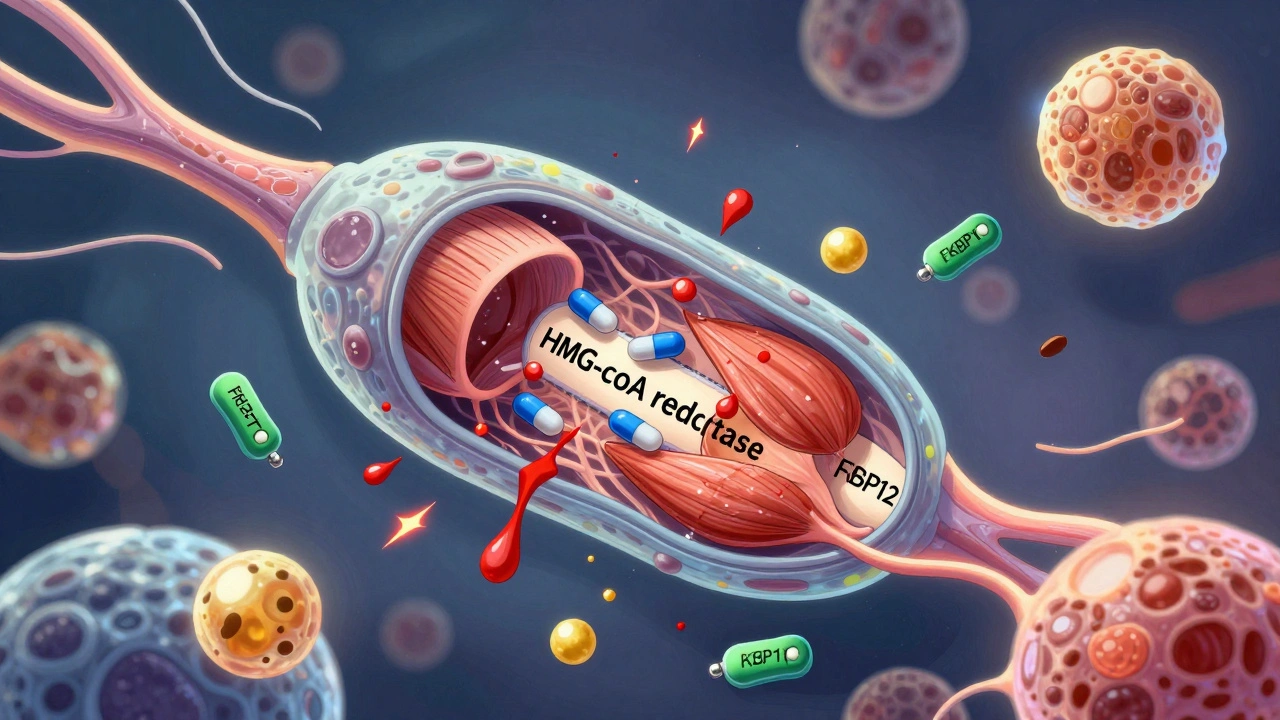
Statins work by blocking HMG CoA reductase, an enzyme in the liver that makes cholesterol. But that same enzyme is also involved in making other essential molecules-ones your muscles need to function properly. When statins interfere, three key things go wrong in your muscle cells.
First, statins cause a protein called FKBP12 to detach from the ryanodine receptor (RyR1), a calcium channel in muscle cells. This isn’t just a small glitch-it’s like removing the safety latch on a spring. Without FKBP12, calcium leaks out of storage in a chaotic way, flooding the muscle cell. This calcium surge activates enzymes that break down muscle tissue and trigger cell death. Studies show this calcium leak increases by more than 200% in people taking statins, and it’s happening right in the skeletal muscle, not the heart.
Second, statins cut production of isoprenoids-farnesyl pyrophosphate and geranylgeranyl pyrophosphate. These molecules are like lubricants for signaling proteins inside cells. Without them, proteins can’t attach properly to cell membranes, and muscle repair signals get scrambled. In lab tests, these compounds drop by 60-80% in muscle tissue after just weeks of statin use.
Third, statins reduce coenzyme Q10 (CoQ10) levels by about 40%. CoQ10 is critical for energy production in mitochondria, the power plants of your cells. When it’s low, muscles tire faster, generate more damaging free radicals, and recover slower. This isn’t just theory-people with statin myopathy often have measurably lower CoQ10 in their muscle biopsies.
Who’s Most at Risk?
Not everyone gets muscle pain on statins. But some people are far more likely to. Age matters-people over 65 are at higher risk. So are those with smaller body frames, kidney or liver problems, or those taking multiple medications. Certain statins are more likely to cause issues. Simvastatin and lovastatin, especially at high doses, carry the highest risk. Atorvastatin and rosuvastatin are generally better tolerated, but they’re not risk-free.
Genetics play a role too. Some people have a variation in the SLCO1B1 gene that makes it harder for their liver to clear statins from the blood. This leads to higher drug levels and more muscle exposure. A simple genetic test can identify this risk before starting treatment.
Then there’s the autoimmune form. In 5-10% of persistent cases, the body starts making antibodies against HMG-CoA reductase-the very enzyme statins block. This rare condition, called anti-HMGCR myositis, can develop even after someone has stopped statins. It’s aggressive, causes severe weakness, and often requires immune-suppressing drugs like prednisone and methotrexate. About 60% of these patients had taken statins before the antibodies showed up.
Real People, Real Symptoms
On Reddit’s r/Statins community, with over 28,000 members, the same stories keep appearing. “Started atorvastatin and couldn’t walk up stairs without pain.” “Felt like I had the flu for six weeks-just muscle aches and exhaustion.” “My doctor said it was ‘just aging,’ but I knew it was the pill.”
A 2021 Healthline survey of 1,245 statin users found that 72% had stopped taking their medication because of muscle symptoms. Nearly half of them tried other cholesterol-lowering drugs. But here’s the catch: 31% of those who kept taking statins despite pain reduced their dose or skipped days. That’s dangerous. Skipping statins raises heart attack risk by 25% over five years, according to the American Heart Association.
One man in Melbourne, 68, started on rosuvastatin after a mild heart attack. Within three weeks, his legs felt heavy. He couldn’t lift his grocery bags. He thought it was arthritis. His GP told him to “push through.” He didn’t. He stopped the statin. His cholesterol jumped back up. He was stuck between a rock and a hard place.
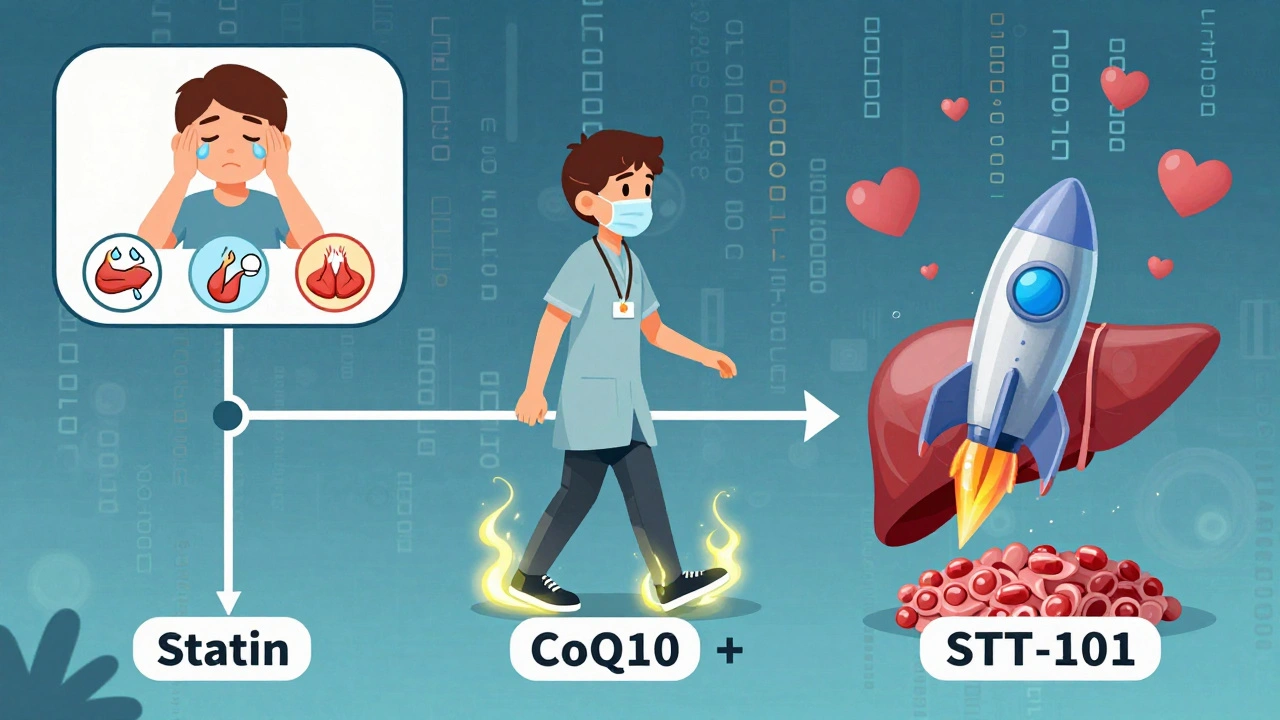
What Works to Fix It
There’s no magic bullet, but there are proven strategies.
First, confirm it’s the statin. Stop the drug for 4 weeks. If your pain fades, it’s likely statin-related. Reintroduce it slowly-sometimes a lower dose works. Switching to a different statin helps 40% of people. Pravastatin and fluvastatin are often better tolerated because they’re less likely to penetrate muscle tissue.
CoQ10 supplementation at 200 mg per day helps about 35% of people in clinical trials. It doesn’t fix everyone, but for those with low muscle CoQ10, it can mean the difference between quitting statins and staying on them. A 2024 study showed that combining CoQ10 with 150 minutes of moderate exercise per week led to 80% symptom resolution-far better than either alone.
Exercise is a game-changer. A Mayo Clinic study found that statin users who walked 30 minutes a day, five days a week, had 41% fewer muscle symptoms than those who didn’t move. Why? Exercise helps FKBP12 reattach to the RyR1 channel, stopping the calcium leak. In rats, voluntary running restored normal calcium control. Human data confirms it.
If those don’t work, switch to non-statin options. Ezetimibe lowers LDL by 15-20% with almost no muscle side effects. PCSK9 inhibitors like evolocumab reduce LDL by 60% and have muscle-related side effects in only 3.7% of users-lower than placebo. The catch? They cost about $5,850 a year, compared to $12 for generic atorvastatin. Insurance often requires failing statins first.
For autoimmune myositis, the path is clear: immunosuppressants. Prednisone and methotrexate bring remission in 68% of cases within six months. But these drugs come with their own risks-bone loss, infection, weight gain. They’re reserved for the most severe cases.
The Bigger Picture
Statins save lives. They prevent heart attacks, strokes, and death. But if you can’t take them, you’re left with fewer options. That’s why new drugs are being developed. Two experimental statins, STT-101 and STT-202, are designed to stay in the liver and avoid muscle tissue. In early tests, they showed 70% less muscle penetration than atorvastatin. If they pass phase III trials, they could change everything.
There’s also a new drug called S107, which locks the RyR1 channel shut, stopping the calcium leak. In a 2023 trial, it cut muscle symptoms by 52%. It’s not approved yet, but it’s a direct fix to the core mechanism.
The message from cardiologists is changing. In 2023, 78% of doctors now talk about muscle pain risks before prescribing statins. Shared decision-making is the new standard. You’re not just a patient-you’re a partner in your care.
What to Do If You’re in Pain
If you’re on a statin and feel new muscle pain:
- Don’t ignore it. Don’t assume it’s just aging or overexertion.
- Track your symptoms: When did they start? Are they worse after activity? Do they improve with rest?
- See your doctor. Ask for a CK (creatine kinase) blood test. Levels over 10x normal mean true myopathy.
- Ask about switching statins or trying a lower dose.
- Request a CoQ10 supplement trial-200 mg daily for 6 weeks.
- Start walking 30 minutes a day, five days a week. It’s not a cure, but it helps.
- If symptoms persist, ask about ezetimibe or a PCSK9 inhibitor.
- If you have severe weakness, trouble standing, or dark urine (a sign of muscle breakdown), go to the ER.
Statin myopathy is real, measurable, and treatable. You don’t have to choose between your heart and your muscles. There’s a path forward-if you know where to look.
Can statins cause permanent muscle damage?
In most cases, no. Muscle symptoms from statins usually resolve within 1 to 4 weeks after stopping the drug. However, in the rare autoimmune form-anti-HMGCR myositis-muscle damage can be severe and persistent without treatment. This form requires immunosuppressive therapy and can lead to long-term weakness if not caught early. Permanent damage is uncommon but possible if muscle breakdown (rhabdomyolysis) is left untreated.
Does CoQ10 really help with statin muscle pain?
Yes, for some people. Clinical trials show that 200 mg of CoQ10 daily reduces muscle pain in about 35% of statin users. It works best when muscle CoQ10 levels are low, which is common with statin use. It’s not a miracle cure, but it’s low-risk and often effective. Many doctors now recommend it as a first step before switching medications.
Can I take statins again after stopping due to muscle pain?
Maybe. About 40% of people who stop statins due to muscle pain can tolerate a different statin at a lower dose. Others can restart the same statin after a break, but at half the original dose. Success depends on the severity of symptoms, the specific statin, and whether you have a genetic risk. Always rechallenge under medical supervision with a CK blood test before and after.
Is exercise safe if I have statin myopathy?
Yes-and it’s recommended. Contrary to old advice, moderate exercise like brisk walking, cycling, or swimming doesn’t worsen statin myopathy. In fact, studies show it helps. Exercise helps restore the FKBP12-RyR1 binding in muscle cells, reducing calcium leaks. People who exercise 150 minutes a week report 41% fewer symptoms. Avoid intense weightlifting or sudden high-intensity workouts until your symptoms improve.
What’s the difference between muscle soreness and statin myopathy?
Normal muscle soreness comes from exercise and fades within a day or two. Statin myopathy is constant, often worse in the thighs and shoulders, and doesn’t improve with rest. It’s not tied to activity-it can happen after sitting for hours. It’s also accompanied by fatigue and weakness, not just pain. If pain starts within the first 6 months of taking a statin and doesn’t match your workout routine, suspect the drug.
Are there natural alternatives to statins?
There are no natural alternatives that match statins’ proven ability to reduce heart attacks and death. Supplements like red yeast rice contain a natural statin (monacolin K) and carry the same muscle risks. Plant sterols, soluble fiber, and omega-3s can help lower cholesterol slightly, but not enough for high-risk patients. If you can’t take statins, prescription non-statin options like ezetimibe or PCSK9 inhibitors are far more effective than supplements.
How do I know if I have the autoimmune form of statin myopathy?
The autoimmune form, anti-HMGCR myositis, is rare but has clear signs: severe, persistent muscle weakness (especially in hips and shoulders), high CK levels even after stopping statins, and symptoms that don’t improve with CoQ10 or rest. A blood test for anti-HMGCR antibodies confirms it. If you’ve had muscle symptoms for more than 6 months after stopping statins, ask your doctor about this test.
What’s Next?
Statin myopathy isn’t going away-but we’re getting better at managing it. The future lies in smarter drugs that target the liver without touching muscle, and in personalized approaches based on genetics, exercise, and supplements. You don’t have to suffer in silence. If your statin is hurting you, there’s a better way. Talk to your doctor. Get tested. Try CoQ10. Move your body. There’s a path that protects your heart without breaking your muscles.


Let’s be real-statins are a corporate scam disguised as medicine. The pharmaceutical industry doesn’t care if you can’t walk; they care if you keep buying pills. They suppress the truth about muscle damage because lawsuits are cheaper than reform. And don’t even get me started on the CoQ10 lie-they won’t tell you it’s been proven for decades, but they’ll sell you the pill for $30 a bottle. Wake up, people.