Stress and Reperfusion Injury Risk Calculator
Your Risk Assessment
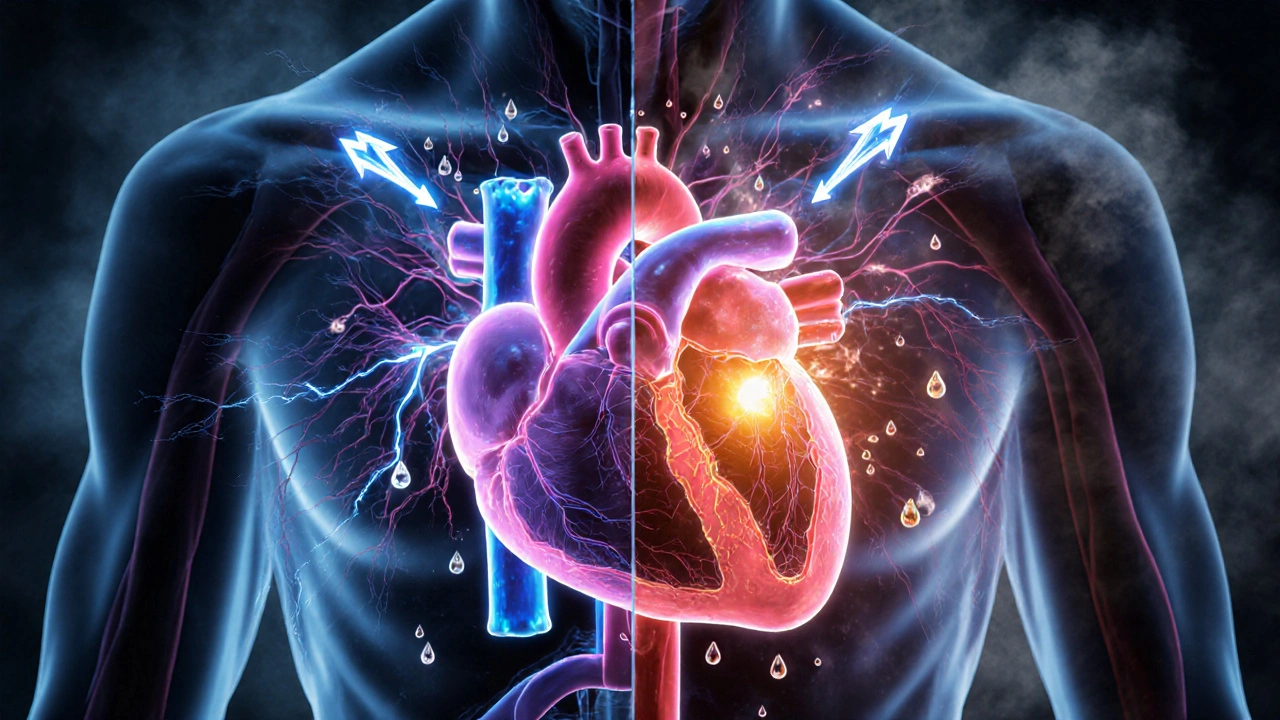
When blood flow returns to tissue after a blockage, reperfusion injury is the damage that occurs because of sudden oxygen influx, inflammatory burst, and metabolic disruption. The problem isn’t just the lack of blood; it’s the shock your cells get when that oxygen rushes back, and stress can turn that shock into a full‑blown crisis.
What is Reperfusion Injury?
Reperfusion injury follows an ischemic episode-think heart attack or stroke-when the blocked artery is opened. The restored blood brings oxygen, but it also delivers reactive oxygen species (highly reactive molecules that damage proteins, lipids, and DNA). Simultaneously, immune cells flood the area, releasing cytokines that amplify tissue damage.
How Stress Enters the Picture
Stress isn’t just a feeling; it’s a cascade of hormones and nervous‑system signals. The sympathetic nervous system (the “fight‑or‑flight” arm of the autonomic nervous system) spikes adrenaline, while the adrenal cortex releases cortisol (a glucocorticoid that mobilises energy and modulates inflammation). Both pathways prime cells for a harsher response when oxygen returns.
Biological Mechanisms Linking Stress to Damage
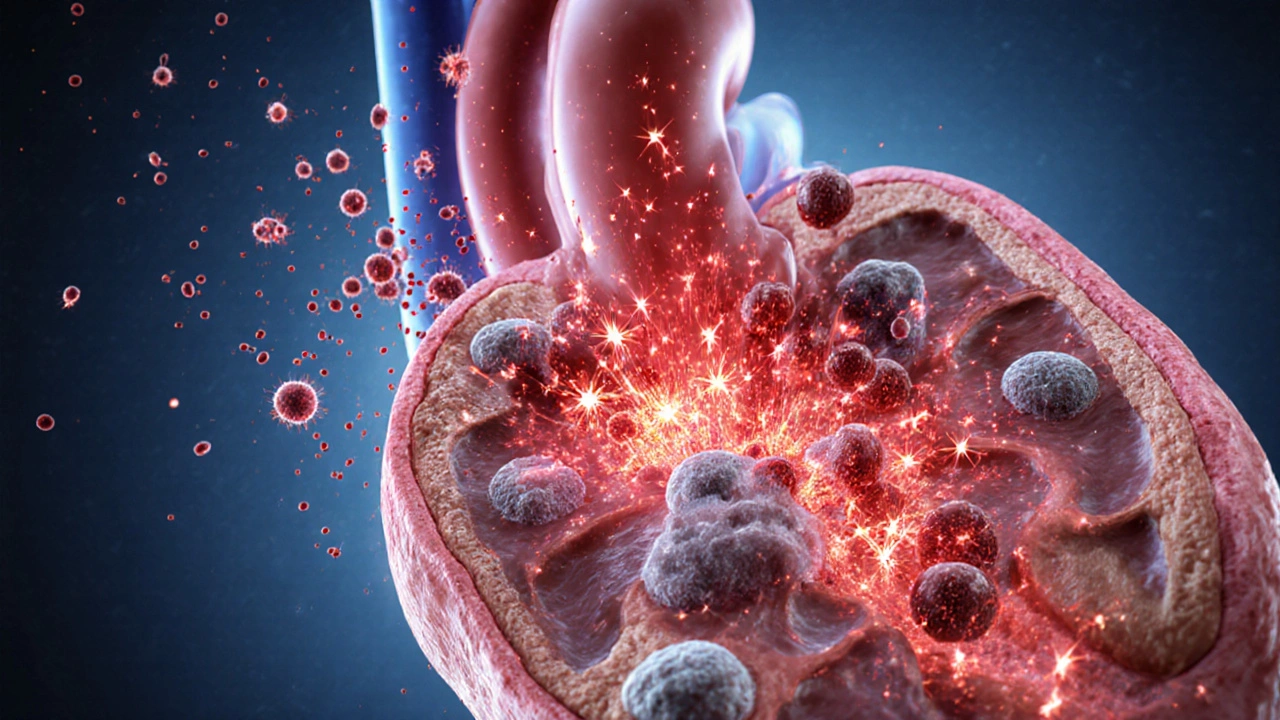
- Oxidative overload: Stress‑induced catecholamines boost mitochondrial activity, generating more ROS. When reperfusion adds its own burst, the antioxidant defenses are quickly overwhelmed.
- Calcium mishandling: Elevated stress hormones increase intracellular calcium, opening the mitochondrial permeability transition pore (a channel that collapses mitochondrial membrane potential and triggers cell death). This accelerates necrosis and apoptosis in the reperfused zone.
- Inflammatory priming: Cortisol, paradoxically, can suppress early anti‑inflammatory pathways while allowing pro‑inflammatory cytokines (IL‑6, TNF‑α) to dominate once blood rushes back.
- Endothelial dysfunction: Stress narrows micro‑vessels via endothelin‑1 release, limiting the gentle wash‑out of debris and prolonging hypoxia even after flow resumes.
Acute vs. Chronic Stress: Different Impacts
| Factor | Acute Stress | Chronic Stress |
|---|---|---|
| Hormone spike | Sharp, short‑lived surge of adrenaline | Persistent elevation of cortisol and catecholamines |
| ROS generation | Transient increase, often mitigated by innate antioxidants | Baseline oxidative load already high, amplifying reperfusion burst |
| Inflammation | Brief, can be protective (pre‑conditioning) | Chronic low‑grade inflammation, worsens cytokine storm |
| Clinical outcome | May limit infarct size if timed correctly | Larger infarct, higher mortality, poorer functional recovery |
Can Stress Be Harnessed? The Paradox of Pre‑conditioning
In controlled settings, brief episodes of stress, such as a short ischaemic clamp or a single dose of adrenaline, trigger protective pathways-heat‑shock proteins, antioxidant enzymes, and nitric‑oxide release. This phenomenon, called ischemic pre‑conditioning (a brief, non‑lethal ischemic event that makes tissue resistant to a later, more severe episode), shows that not all stress is harmful. The key is timing and magnitude; too much or sustained stress flips the switch toward injury.
Therapeutic Strategies to Counter Stress‑Driven Damage
- Beta‑blockers: By dampening sympathetic output, they lower heart rate, reduce calcium influx, and blunt ROS spikes.
- Glucocorticoid modulation: Low‑dose steroids administered shortly before reperfusion can temper the inflammatory surge without aggravating hyperglycaemia.
- Antioxidant therapy: Agents like N‑acetylcysteine replenish glutathione, directly scavenging ROS generated by both stress and reperfusion.
- mPTP inhibitors: Drugs such as cyclosporine A keep the mitochondrial pore closed, preserving ATP production during the oxidative onslaught.
- Stress‑reduction techniques: Mindfulness, controlled breathing, and short‑term exercise improve autonomic balance, lowering baseline catecholamine levels before any cardiac event.
Key Takeaways
- Reperfusion injury is a double‑edged response to restored blood flow, driven largely by ROS and inflammation.
- Both acute and chronic stress amplify oxidative and inflammatory pathways, but acute, well‑timed stress can pre‑condition tissue.
- Managing sympathetic activity, cortisol spikes, and mitochondrial stability are central to limiting damage.
- Pharmacologic tools (beta‑blockers, antioxidants, mPTP inhibitors) work best when combined with lifestyle stress‑management.
- Future research is honing personalized stress‑modulation protocols to improve outcomes after heart attacks and strokes.

Frequently Asked Questions
Why does the sudden return of blood cause more damage than the blockage itself?
When oxygen floods previously starved cells, it reacts with accumulated electrons in mitochondria, creating a burst of reactive oxygen species. Those ROS attack membranes, proteins, and DNA, while the sudden influx also draws immune cells that release inflammatory cytokines, together magnifying tissue injury.
Can everyday stress (like a tough day at work) affect heart‑attack outcomes?
Chronic psychosocial stress raises baseline cortisol and catecholamine levels, which prime the heart for a larger oxidative surge during reperfusion. Studies show higher long‑term stress correlates with bigger infarct sizes and slower recovery after a heart attack.
Is there a safe way to use stress as a protective pre‑conditioning tool?
Medical pre‑conditioning typically uses brief, controlled periods of ischemia (e.g., inflating a blood‑pressure cuff for a few minutes) rather than exposing patients to real stress. Experimental protocols with low‑dose adrenaline have shown benefit, but they must be tightly regulated and are not yet standard clinical practice.
What role do antioxidants play during reperfusion?
Antioxidants such as N‑acetylcysteine replenish intracellular glutathione, neutralising the surge of ROS. Clinical trials suggest they can reduce infarct size when given just before re‑establishing blood flow, especially in patients with high baseline oxidative stress.
Are there any emerging therapies targeting the mitochondrial pore?
Yes. New selective mPTP inhibitors are being tested in phase‑II trials. They aim to keep the pore closed during the critical minutes of reperfusion, preserving ATP production and preventing cell death.


Great overview on how stress intersects with reperfusion injury. The way you broke down oxidative overload and calcium mishandling makes the mechanisms much clearer. I especially appreciated the table comparing acute and chronic stress-it highlights the clinical relevance nicely. It’s also helpful to see the therapeutic options laid out in a stepwise fashion. Overall, this synthesis is both informative and accessible for readers from different backgrounds.