Most people think a few weird patches on their skin are just a sunburn or a rash that’ll fade. But if you’ve got white, pink, or brown spots on your chest, back, or shoulders that don’t go away - especially if they’re scaly and show up every summer - it might be tinea versicolor. It’s not a bug you caught from someone else. It’s not caused by dirt. It’s your own skin yeast going rogue.
What’s Really Happening on Your Skin?
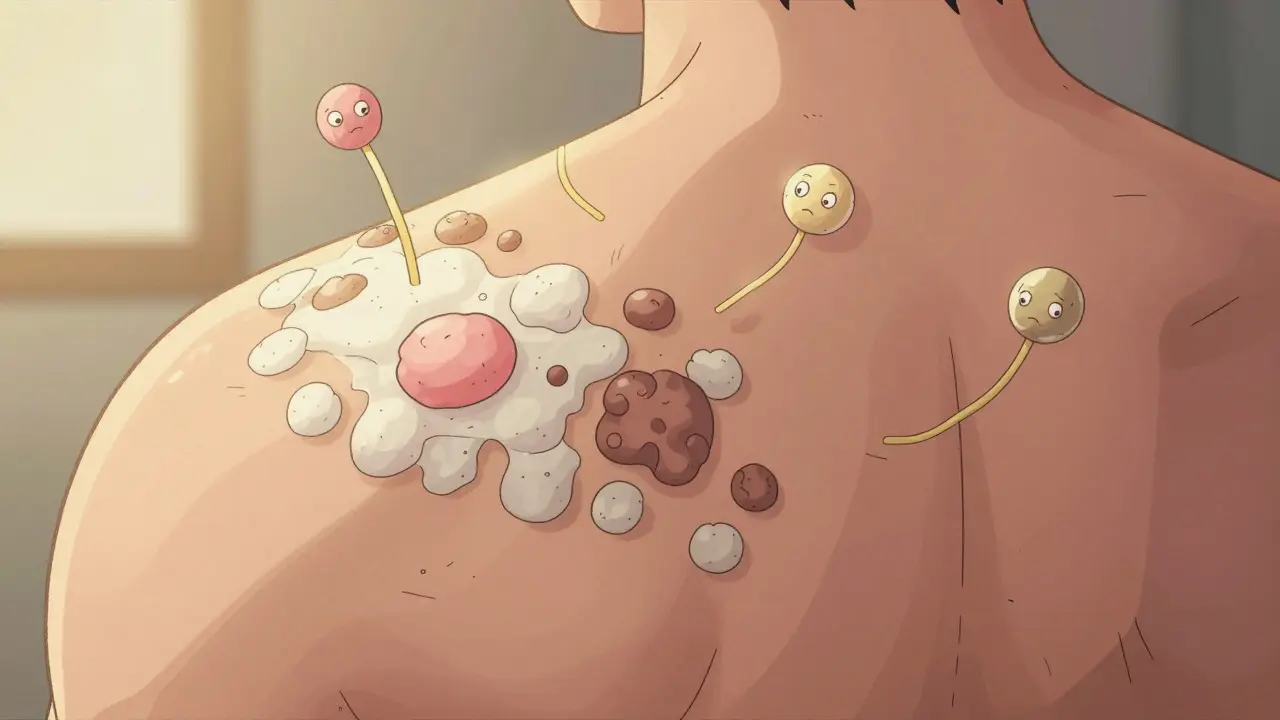
Tinea versicolor is caused by Malassezia yeast - a type of fungus that lives on everyone’s skin. Normally, it’s harmless. But when conditions get warm, sweaty, and oily, this yeast starts multiplying fast. It doesn’t invade deep into your skin. It just hangs out on the surface and starts messing with your pigment.
That’s why you see patches. In lighter skin tones, they often look white or pink. In darker skin, they can appear darker or lighter than the surrounding skin. The yeast produces azelaic acid, which blocks melanin production. So the affected areas don’t tan like the rest of your skin. That’s why they stand out so much in summer - your healthy skin darkens, and the infected patches stay pale.
It’s most common in teens and young adults, mostly because their skin produces more oil. But it can hit anyone, especially if they live in hot, humid places. In tropical regions, up to half the population deals with it at some point. Even in Melbourne, where summers are warm and sticky, it’s not rare.
How Do You Know It’s Tinea Versicolor?
Doctors don’t guess. They look. A quick scrape of the patch with a wooden stick and a drop of potassium hydroxide (KOH) under a microscope shows the classic "spaghetti and meatballs" pattern - long threads (hyphae) and round yeast cells. That’s 95% accurate.
You won’t see this on your face unless you’re a child. It mostly shows up on the chest, back, neck, and upper arms. It doesn’t itch much, if at all. No pus, no blisters, no pain. Just patches that look off and won’t tan. If you’ve been told it’s eczema or psoriasis and nothing’s worked - this could be it.
And no, it’s not contagious. You can’t catch it from towels, gym equipment, or your partner. That’s a myth that causes unnecessary shame. People avoid swimming pools, skip beach trips, wear high-neck shirts in summer - all because they think it’s catching. It’s not.
Treatment: What Actually Works
You don’t need a prescription to start. The first-line fix is over-the-counter selenium sulfide shampoo - the kind you’d use for dandruff. Selsun Blue, for example. Apply it to the affected areas and leave it on for 10 minutes, then rinse. Do this once a day for two weeks. Studies show it clears the infection in about 78% of cases.
Or try ketoconazole shampoo (Nizoral). Same method. Leave it on 5-10 minutes, rinse. It’s just as effective. Both work by killing the yeast on the surface.
If that doesn’t cut it, or the patches are widespread, your doctor might prescribe oral fluconazole. One 300mg pill once a week for two to four weeks clears it in over 90% of cases. But it’s not casual. Fluconazole can affect your liver, so blood tests are needed before and after. It’s not something to take without supervision.
Topical creams like clotrimazole or miconazole? They help, but they’re messy. You’d need to cover every patch, every day, for weeks. Shampoos are easier. You can wash your whole chest and back in the shower. That’s why most dermatologists recommend them first.

The Big Problem: It Comes Back
Here’s the hard truth: 60 to 80% of people get it again within a year. That’s not because treatment failed. It’s because the yeast never left. It’s always there. You just suppressed it.
So treatment isn’t just about clearing the patches. It’s about preventing them from coming back. And that’s where most people drop the ball.
UCLA Health did a study with 200 patients. Those who used ketoconazole shampoo once a month - even after the patches were gone - cut their recurrence rate to 25% in a year. Those who stopped? Almost all had it return.
That’s the secret. Maintenance. Not just treatment.
How to Prevent Recurrence - The Real Rules
Here’s what actually works, based on real clinical data and patient outcomes:
- Use antifungal shampoo monthly - Even in winter. Pick one day each month (like the first Sunday) and wash your chest, back, and shoulders with ketoconazole or selenium sulfide shampoo. Leave it on for 10 minutes. Rinse. Do this for at least 6 months after your last outbreak. If you’ve had three or more recurrences, keep doing it year-round.
- Avoid oily products - Heavy lotions, sunscreen with mineral oil, hair gels, or face oils can feed the yeast. Switch to water-based moisturizers and oil-free sunscreens. Look for "non-comedogenic" on the label.
- Wear breathable clothes - Tight, synthetic fabrics trap sweat. Cotton, bamboo, or moisture-wicking athletic wear helps. After sweating, change clothes within an hour. Don’t sit in damp gym gear.
- Don’t over-cleanse - Scrubbing with harsh soaps or antibacterial washes kills good bacteria that keep yeast in check. Use a gentle, pH-balanced cleanser. Your skin doesn’t need to be squeaky clean.
- Watch the heat and humidity - If you’re in a hot climate or spend a lot of time in saunas, steam rooms, or tropical vacations, be extra careful. The yeast thrives there. Use your shampoo more often during those months.
And yes - sun exposure makes it worse. Not because the sun causes it, but because your healthy skin tans and the infected patches don’t. That contrast makes them glaring. Use sunscreen every day, even if you’re not at the beach. It helps even out your skin tone over time.
What Doesn’t Work
There’s a lot of misinformation out there.
Apple cider vinegar? Tea tree oil? Lemon juice? Some people swear by them. But there’s zero clinical proof they kill Malassezia yeast effectively. They might irritate your skin, making things worse.
Antibiotics? No. This is a fungus, not a bacteria. Antibiotics won’t touch it.
And please - don’t blame yourself. It’s not because you’re dirty. It’s not because you didn’t shower enough. Even athletes, doctors, and people who bathe twice a day get it. It’s about your skin’s chemistry, your environment, and your immune system’s response. Nothing to be ashamed of.

How Long Until Your Skin Looks Normal Again?
This is where people get frustrated. Even after the yeast is gone, the patches can stick around for months. Your skin needs time to produce pigment again. In 41% of cases, it takes 6 to 12 months for color to return fully.
Don’t panic. Don’t re-treat. Just be patient. Keep using your monthly shampoo. Keep wearing sunscreen. Your skin will catch up. If you keep re-treating too soon, you risk irritating your skin and triggering another flare.
One patient on RealSelf.com said: "It’s been two years since I was treated, and my back still doesn’t tan evenly. I avoid the beach." That’s heartbreaking - and unnecessary. With time and consistent care, most people see full pigment recovery.
When to See a Dermatologist
You don’t need to see one right away if you’re just starting out. Try the shampoo routine first. But if:
- The patches spread quickly
- You’ve had three or more recurrences in a year
- It’s not improving after 4 weeks of treatment
- You have other health issues like diabetes, HIV, or are on steroids
Then get checked. You might need oral medication. Or your doctor might test for something else - like pityriasis rosea or eczema, which can look similar.
Also, if you’re emotionally stressed by it - if you’re avoiding social situations, feeling anxious about your appearance - talk to someone. Studies show 37% of people with tinea versicolor report significant emotional distress. You’re not alone. Support groups like the American Academy of Dermatology’s Versicolor Support Network have helped over 12,500 people just like you.
What’s Next? The Future of Treatment
Researchers are looking into probiotics - good bacteria that might naturally keep Malassezia in check. Early lab studies show certain strains can suppress the yeast by 68%. That’s promising. But it’s still years away from being available to the public.
Another concern: some strains of yeast are becoming less sensitive to ketoconazole. About 8.7% of recurrent cases now show reduced response. That’s why doctors are starting to recommend combination therapies - using two types of antifungals together. Clinical trials are underway, but for now, the old-school monthly shampoo is still the gold standard.
The bottom line? Tinea versicolor is annoying, persistent, and frustrating - but it’s not dangerous. It’s manageable. And with the right routine, you can keep it away for good.
Start with the shampoo. Stick with the monthly use. Avoid oils and sweat traps. Be patient with your skin. And remember - you’re not broken. Your skin just has a yeast that likes warm weather. And now you know how to handle it.


It’s wild how something so common gets turned into a shame spiral. I had this for years and thought I was dirty because my skin looked weird. Turns out, my skin just likes to throw parties when it’s hot. No judgment, no panic - just a monthly shampoo and a lot of sunscreen. I stopped avoiding the beach. My back still doesn’t tan evenly, but I don’t care anymore. It’s just skin.