Every day, millions of Americans take generic drugs instead of brand-name medications. They do it because generics cost less-often 80% to 85% less. But a common question lingers: Do generic drugs really work the same? The answer isn’t guesswork. It’s science, enforced by the U.S. Food and Drug Administration (FDA) through one of the most rigorous drug approval systems in the world.
The FDA’s Secret: The ANDA Process
The FDA doesn’t require generic drug makers to repeat the same expensive clinical trials that brand-name companies ran. Instead, they use a shortcut called the Abbreviated New Drug Application, or ANDA. This isn’t a loophole-it’s a carefully designed system created by the Hatch-Waxman Act of 1984. The law balanced two goals: letting patients access affordable medicine, while still protecting the innovation that led to the original drug. To get approved, a generic manufacturer must prove their product is identical to the brand-name drug in three critical ways: active ingredient, strength, and how it’s taken (like tablet, capsule, or injection). The brand-name drug is called the Reference Listed Drug, or RLD. Every generic must match it exactly in these areas.Bioequivalence: The Science Behind the Match
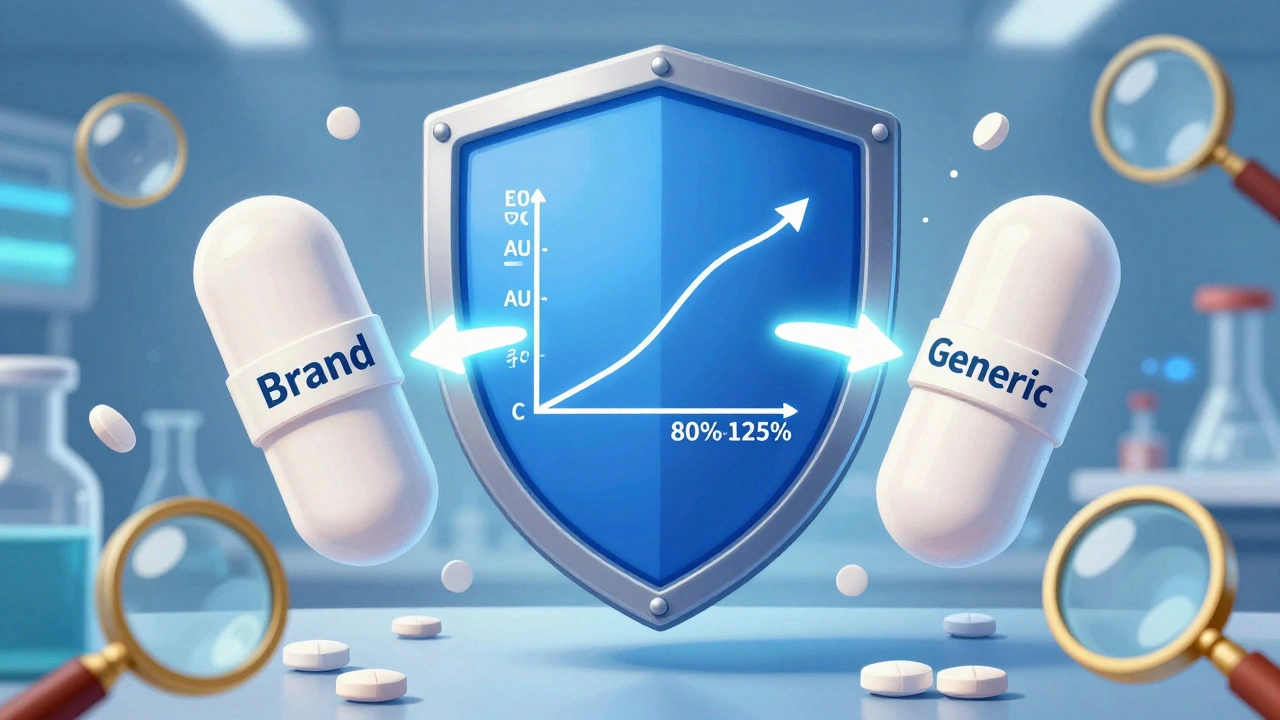
The biggest concern people have is whether the generic gets into the bloodstream the same way. That’s where bioequivalence comes in. The FDA requires generic drugs to deliver the same amount of active ingredient at the same rate as the brand. How do they measure this? In clinical studies, 24 to 36 healthy volunteers take both the brand and generic versions under controlled conditions. Blood samples are taken over time to track how much of the drug enters the bloodstream and how fast. The key numbers? The area under the curve (AUC) and the maximum concentration (Cmax). For the generic to be approved, these values must fall within 80% to 125% of the brand’s results. That’s not a wide range-it’s tight. The 90% confidence interval for both AUC and Cmax must stay inside those bounds. This isn’t just theory. The FDA publishes specific bioequivalence guidelines for over 1,500 drugs. For example, if you’re making a generic version of metformin, they’ll tell you exactly how many people to test, whether they should fast or eat before taking the pill, and which blood tests to use. There’s no room for guesswork.Manufacturing: Same Rules, No Exceptions
It’s not enough for the drug to work the same in a lab. The factory that makes it must be just as precise. Every generic drug plant, whether it’s in the U.S., India, or Germany, must follow Current Good Manufacturing Practices (cGMP). That means:- Each batch must have the same strength, purity, and quality as the last
- Equipment is cleaned and tested to prevent contamination
- Every tablet must contain between 85% and 115% of the labeled amount of active ingredient

Why Some People Still Doubt
Despite all this, some patients report feeling different on a generic. You might hear stories on Reddit or from friends: “My generic for thyroid medication didn’t work like the brand.” Or, “I switched to the cheaper version and got headaches.” These reports aren’t ignored. The FDA takes them seriously. For drugs with a narrow therapeutic index-like warfarin, levothyroxine, or phenytoin-where even a small change in blood level can cause harm or failure-the FDA demands stricter bioequivalence standards: 90% to 111% instead of 80% to 125%. They’ve also created a public list of these high-risk drugs so doctors and pharmacists know which ones need extra caution. A 2020 study in JAMA Internal Medicine found that 11% of doctors still had concerns about switching patients on narrow-index drugs. But here’s the key: those concerns didn’t come from evidence of harm. They came from caution. And the FDA’s rules are designed to reduce that caution over time.Real-World Data: Do Generics Actually Work?
The best proof isn’t in lab reports-it’s in real lives. A 2023 analysis of 15 million patient records by IQVIA looked at 20 common medications, including atorvastatin (for cholesterol) and metformin (for diabetes). The results? No meaningful difference in outcomes between brand and generic. In fact, patients were 3.2% more likely to keep taking their generic because it cost less. The FDA’s own adverse event database shows the same number of reported side effects per million prescriptions for generics and brands. That’s a powerful stat. If generics were causing more problems, you’d see it here. Pharmacists-who see patients daily-confirm this. In a 2022 Reddit thread with 147 pharmacist comments, 82% said they saw no clinical difference. The rest noted rare cases with complex forms like inhalers or topical creams, where delivery matters more. Even then, the issue wasn’t the drug itself-it was how it was made.What Happens When a Generic Gets Rejected?
Not every application gets approved. In 2022, about 35% of ANDA submissions were refused right away because they were incomplete or poorly organized. The FDA doesn’t waste time on sloppy paperwork. Of the applications that make it to full review, the most common reasons for rejection are:- Inadequate bioequivalence data (28%)
- Manufacturing flaws (22%)
- Labeling errors (18%)

Who Makes These Drugs-and Why It Matters
You might think big companies like Pfizer or Merck make all the generics. They don’t. In fact, 55% of generic approvals go to smaller manufacturers. The FDA’s Generic Drug Competition Action Plan, started in 2017, was designed to encourage more players to enter the market. Why? More competition means lower prices. The top three generic makers in the U.S. are Teva, Viatris, and Sandoz. But thousands of other companies-many based overseas-also produce FDA-approved generics. That’s why the FDA inspects facilities around the world. They don’t care where the drug is made. They care that it meets U.S. standards.The Future: Faster, Smarter, Broader
The FDA is pushing to make the process even better. Under GDUFA III, which runs through 2027, they’re aiming to cut review times to 8 months for standard applications and 6 months for priority ones. They’re also creating new pathways for complex generics-like biosimilars, which are generic versions of biologic drugs (think insulin or cancer treatments). The first guidances for these are expected in 2024. They’re also speeding up approvals for drugs that are in short supply. In 2023, 47 products got fast-track status. Twelve of them were approved in under six months-half the normal time.Bottom Line: You Can Trust the Generic
The FDA doesn’t approve a generic drug because it’s cheaper. They approve it because it works just as well. Every step-from the chemistry to the clinical trial to the factory inspection-is designed to prove that. And the data backs it up: millions of patients use generics every day without issue. If your doctor prescribes a generic, or your pharmacist swaps your brand for a cheaper version, you’re not taking a risk. You’re taking a scientifically validated, cost-saving, FDA-approved medicine. The system isn’t perfect, but it’s built on evidence, not luck.Are generic drugs as effective as brand-name drugs?
Yes. The FDA requires generic drugs to have the same active ingredient, strength, dosage form, and route of administration as the brand-name version. They must also prove bioequivalence-meaning they deliver the same amount of drug into the bloodstream at the same rate. Clinical studies and real-world data show no meaningful difference in effectiveness for the vast majority of medications.
Why do some people say generics don’t work for them?
Some patients report feeling different after switching, especially with drugs that have a narrow therapeutic index, like thyroid medication or blood thinners. While the FDA requires stricter bioequivalence standards for these drugs (90-111% instead of 80-125%), individual sensitivity or placebo effects can cause perceived differences. These reports are rare and rarely backed by clinical evidence. If you notice a change, talk to your doctor-but don’t assume the generic is faulty.
Do generic drugs have the same side effects as brand-name drugs?
Yes. Since the active ingredient is identical, the side effect profile is the same. The FDA’s Adverse Event Reporting System shows that the rate of side effects per million prescriptions is statistically identical between generics and brand-name drugs. Differences in inactive ingredients rarely cause new side effects, and when they do, they’re mild and uncommon.
How does the FDA ensure quality across different manufacturers?
Every manufacturing facility-domestic or international-must pass FDA inspections under Current Good Manufacturing Practices (cGMP). The FDA inspects these sites regularly and without notice. If a plant fails to meet standards, the FDA can refuse approval or even ban imports. Batch-to-batch consistency is monitored using strict quality control standards, including content uniformity tests that require each tablet to contain 85-115% of the labeled active ingredient.
Can I trust generics from other countries?
Yes-if they’re sold in the U.S. The FDA inspects foreign manufacturing sites just like U.S. ones. Over half of all generic drugs sold in the U.S. are made overseas, mostly in India and China. The FDA has offices in those countries to conduct inspections. If a drug is approved and sold in the U.S., it meets the same standards as a brand-name drug, no matter where it was made.
Why are generic drugs so much cheaper?
Generic manufacturers don’t have to repeat the costly clinical trials that brand-name companies did. They rely on the FDA’s previous findings of safety and effectiveness. This cuts development time and cost significantly. While developing a generic can still cost $1.5 million to $3 million, it’s far less than the $1 billion+ it often takes to bring a new brand-name drug to market. Competition among multiple generic makers also drives prices down.
What’s the difference between an ANDA and an NDA?
An NDA (New Drug Application) is submitted by the original brand-name drug maker and includes full data from preclinical and clinical trials to prove safety and effectiveness. An ANDA (Abbreviated New Drug Application) is for generics and relies on the FDA’s prior approval of the brand-name drug. Generic applicants only need to prove bioequivalence and manufacturing quality, not re-prove safety and efficacy.
Are there any drugs that shouldn’t be switched to generics?
For most drugs, switching is safe and effective. But for drugs with a narrow therapeutic index-like warfarin, levothyroxine, phenytoin, and lithium-the FDA recommends extra caution. These drugs require tighter bioequivalence standards (90-111%) and close monitoring by a doctor. Even then, the FDA approves generics for these drugs when they meet the stricter criteria. Always consult your doctor before switching, especially if you’re on a complex medication.


I switched my thyroid med to generic last year and was terrified-but zero issues. Seriously, my energy’s back, no headaches, no weird vibes. The FDA’s got this locked down.
❤️